Secondary sexual characteristics were normal. Further questioning revealed that he had previously undergone paediatric surgical intervention, although the exact nature of this was lacking in detail. The assumption was that this was probably previously failed attempts at bilateral orchidopexy and at some point, the patient had subsequently been lost to follow-up. He had no children and denied having any particular concerns regarding his UDT, although on specific questioning he was aware of a relatively low libido and limited erectile function. Interestingly, family history inquiry revealed a similar history of UDT in the patient’s brother who was also on testosterone hormone replacement therapy.
Regarding the ureteric stone, this was managed conservatively; the stone passed spontaneously without the need for intervention. On closer review of the CT KUB however, there was an organ identified superior to the bladder which appeared to be consistent with a uterus (Figures 1&2). An MRI scan was therefore undertaken, firstly to investigate the uterine mass further and secondly to identify any gonadal tissue.

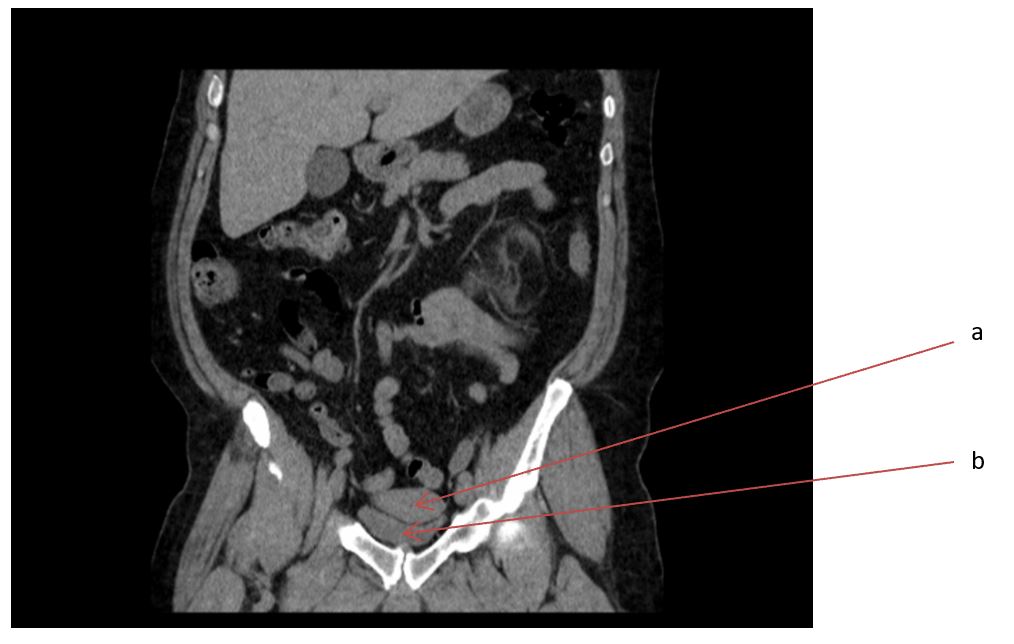
The MRI confirmed a normal prostate and seminal vesicles along with the presence of a soft tissue structure consistent with a uterus (Figure 3). Presumed gonadal tissue was seen bilaterally (Figure 4). The hormonal screen revealed features of primary hypogonadism with a low serum testosterone of 1.8nmol/L and elevated FSH and LH levels. Karyotyping revealed a normal male karyotype 46, XY. Input from the endocrinologist was sought regarding the need for testosterone replacement and detailed discussions with the patient were undertaken on several occasions regarding the diagnosis and treatment options.
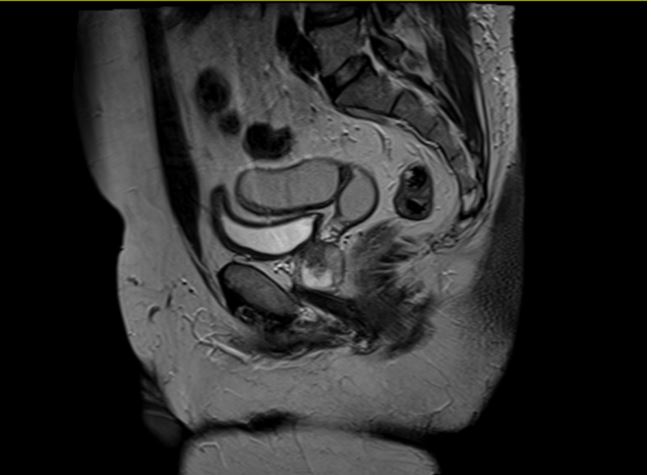
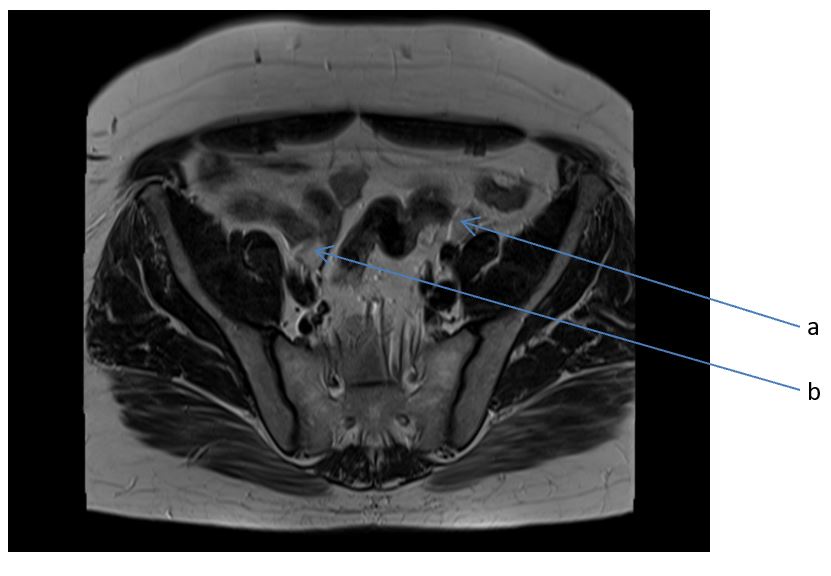
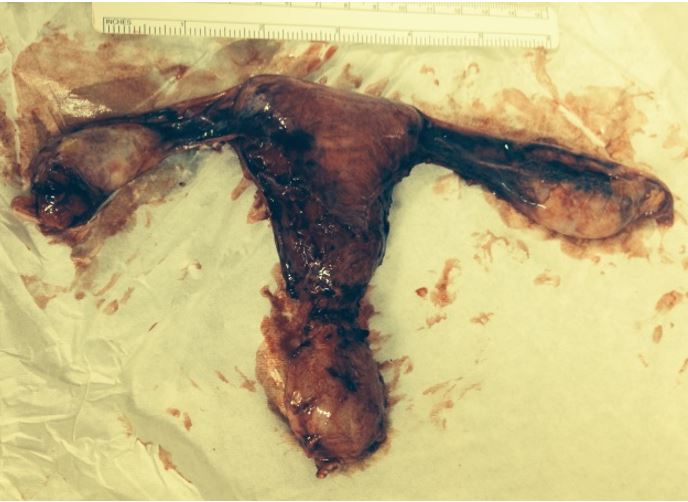
Following discussions with both urology and endocrinology the patient elected to undergo surgical excision. Intraoperatively, laparoscopy confirmed a pelvic structure posterior to the bladder and anterior to the recto-sigmoid junction with the macroscopic appearance of a uterus and broad ligament-like structures attached to bilateral testes. The patient underwent robotic-assisted excision of Müllerian duct remnant and bilateral excision of intra-abdominal testes on 21st January 2015 by a standard 6 port transperitoneal approach with da Vinci Si system. There were no complications and the patient had an unremarkable post-operative recovery being discharged on the first postoperative day.
Histological analysis confirmed a primitive uterus with pathological features of cervical glandular morphology and a combination of spermatic cord and fallopian tube encased within a single sheath bilaterally. Both gonads showed complete atrophy of the seminal tubules with streak testes. There was also Leydig cell hyperplasia but no evidence of testicular malignancy.
The patient was subsequently reviewed in a clinic and made a full recovery from the surgical procedure. He was been commenced on testosterone replacement and discharged from urological follow-up. Ongoing follow is under the care of the endocrinologist.
PMDS is a rare form of internal male pseudohermaphroditism in which Müllerian duct derivatives are seen in a male patient. This syndrome is characterized by the persistence of Müllerian duct derivatives (i.e. uterus, cervix, fallopian tubes and upper two-thirds of the vagina) in a phenotypically and karyotypically male patient. The syndrome is caused either by an insufficient amount of Müllerian inhibiting factor (MIF) or due to the insensitivity of the target organ to MIF. The evidence base for the management of adults with PMDS is limited but in general surgical excision of the remnant is recommended due to the risk of malignant transformation both in the uterus and gonads.
The literature regarding management mainly consists of case reports reporting laparoscopic removal of the remnants in infants. We present an interesting clinical case presenting in adulthood where the patient underwent a robotic-assisted excision of the remnants. To our knowledge, this is a novel technique following which the patient made an excellent recovery.
Written By: Alastair D'Oyley, MD, Victoria Louise Lavin, MD, Mark Ian Johnson, MD, FRCS, S.Venkatesan, Greta Rodrigues, MD, Srinivas Annavaparu, MBBS, MD, DNB, DipFMS, FRCPath, Departments of Urology and Histopathology, Freeman Hospital, Newcastle upon Tyne, United Kingdom
References:
1. RS Kamble, RK Gupta, AR Gupta, PR Kothari, KV Dikshit, and KK Kesan, Laparoscopic management of transverse testicular ectopia with persistent mullerian duct syndrome, J Minim Access Surg. 2015 Jul-Sep; 11(3): 213–215. doi: 10.4103/0972-9941.152093
2. Shalaby MM, Kurkar A, Zarzour AA, Faddan AA, Khalil M and Abdelhafez MF, The Management of Persistent Mullerian Duct Syndrome, Arab J Urol. 2014 Sep;12(3):239-44. doi: 10.1016/j.aju.2014.04.001. Epub 2014 Apr 26
3. Farikullah J1, Ehtisham S, Nappo S, Patel L, Hennayake S., Persistent Müllerian duct syndrome: lessons learned from managing a series of eight patients over a 10-year period and review of literature regarding malignant risk from the Müllerian remnants., BJU Int. 2012 Dec;110(11 Pt C):E1084-9. doi: 10.1111/j.1464-410X.2012.11184.x. Epub 2012 Apr 30.
4. Wu JA, Hsieh MH., Robot-assisted laparoscopic hysterectomy, gonadal biopsy, and orchiopexies in an infant with persistent mullerian duct syndrome.,Urology. 2014 Apr;83(4):915-7. doi: 10.1016/j.urology.2013.10.006. Epub 2013 Nov 15.
5. Manjunath BG1, Shenoy VG, Raj P., Persistent müllerian duct syndrome: How to deal with the müllerian duct remnants - a review. Indian J Surg. 2010 Feb;72(1):16-9. doi: 10.1007/s12262-010-0003-x. Epub 2010 Feb 5.


