Low regional urologist density has been linked to larger stone burden at presentation to tertiary referral centers and higher urologic cancer mortality rates. However, the financial consequences of poor access to urologic care have not been explored.
This study utilizes the Registry of Stones of the Kidney and Ureter (ReSKU) database at the Universit of California San Francisco (UCSF) and specific hospital cost data to investigate this issue. We found that when controlling for other markers of low socioeconomic status, medical comorbidities, stone size, stone complexity, and surgical approach, living in a county with low urologist density predicted higher costs of stone surgery. When looking at the differences between patients from high and low urologist density counties, patients from low urologist density counties had almost double the rate of prolonged hospitalization and surgical complications, likely explaining higher costs for these patients.
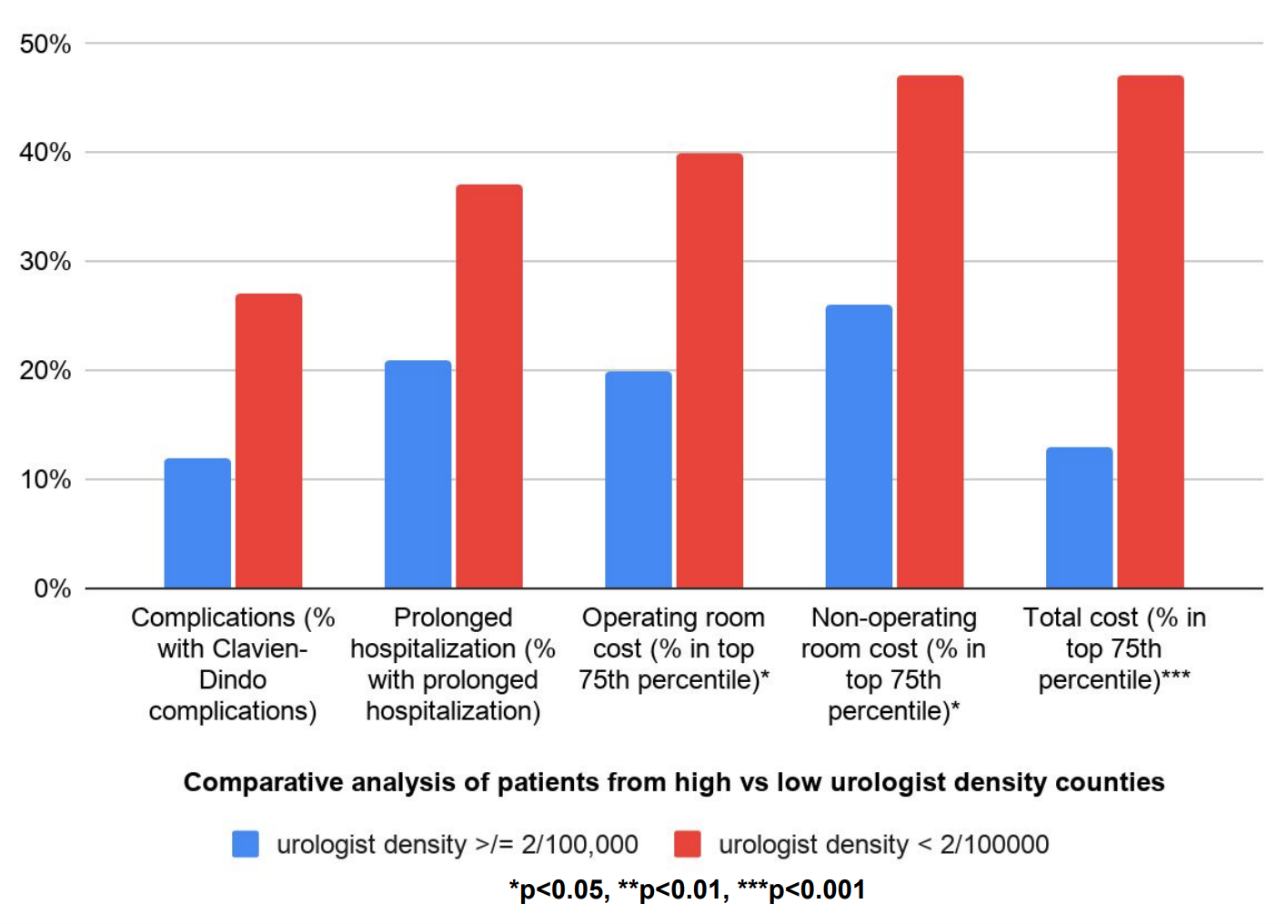
We suspect that low urologist density by county is a marker of reduced overall regional access to health care. Indeed, these patients were more likely to be underinsured, had higher ASA scores, and had higher rates of diabetes, hypertension, and obesity. Although differences in these categories were not statistically significant, they do suggest that patients from low urologist density counties have less effective overall preventative care and chronic disease maintenance. This would explain the higher rates of complications, prolonged hospitalization, and cost in patients from low urologist density counties. Therefore, improving overall access to health care in high-risk populations may reduce surgical costs of stone disease and other surgical diseases as well.

Written by: David Bayne, MD, MPH, Assistant Professor, Department of Urology, University of California San Francisco, San Francisco, California
Read the Abstract


