The most frequently reported complications of URS are ureteral wall injury, stone migration, and ureteral stent discomfort.5 The most severe complications include multi-organ failure, urosepsis, and death.5 The rates of these severe complications vary substantially between studies and may be underreported.5 Urosepsis is sepsis originating from the urogenital tract.7 Sepsis is a clinical syndrome consisting of physiologic abnormalities caused by a host response to an infection and may lead to multiple organ dysfunction syndrome and, death.7 We conducted a systematic review and meta-analysis to quantify the risk of postoperative urosepsis after URS for stone disease and to identify the potential risk factors for this complication.4 In 13 studies (5 prospective) with 5,597 patients, the pooled incidence of postoperative urosepsis was 5.0% (Figure).
Figure. Forest Plot of Postoperative Urosepsis Risk in Patients Undergoing URS.

Source: Bhojani N, et al. J Endourol. 2021;10.1089/end.2020.1133.
The postoperative urosepsis rate and 95% CI are plotted for each study. The pooled mortality rate (diamond apex) and 95% CI (diamond width) are calculated using a random effects model. Pooled urosepsis risk = 5.0%. Heterogeneity: I2 = 95%; p < 0.001. CI = confidence interval; ES = Effect Size.\
One of the key findings of this meta-analysis was that the incidence rates for urosepsis varied extensively between studies. It is possible that many urologists may not be aware of the high incidence rate for urosepsis since standardized reporting systems are seldom used, postoperative management of this condition may occur in a different setting of care (onset of the condition may be 1-2 days later), and misdiagnosis may occur (i.e., cystitis). A recently published literature review (n=187 studies) by De Coninck and colleagues (2021) examining all complications associated with URS found that severe complications such as urosepsis may be underreported worldwide and may give urologists an “unwarranted sense of security when performing a URS.”5 These findings underscore the importance of risk stratification of patients in the pre-operative and perioperative settings as well as post-operative surveillance.
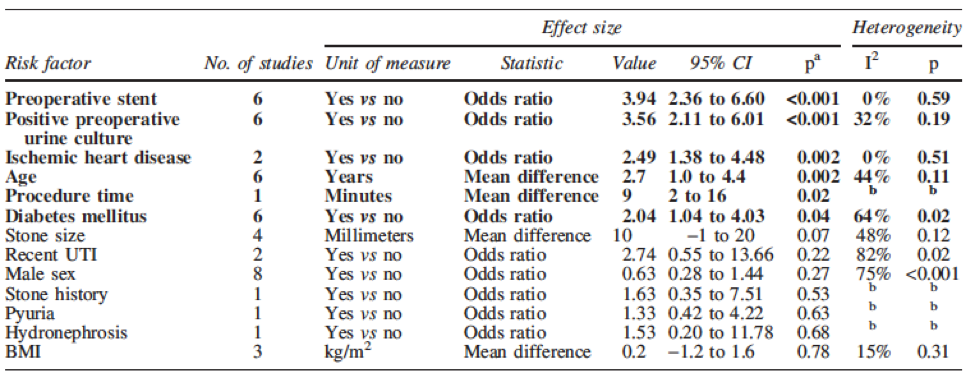
Our study also identified six factors that were statistically associated with increased postoperative urosepsis risk: older age, comorbidities such as diabetes mellitus and ischemic heart disease, preoperative stent placement, positive preoperative urine culture (indicative of infection), and longer procedure time (Table).
Table. Summary of Risk Factors for Postoperative Urosepsis in Patients Undergoing URS for Stone Disease
Source: Bhojani N, et al. J Endourol. 2021;10.1089/end.2020.1133.
This information is important for urologists as it can assist with preoperative risk stratification before ureteroscopic procedures and also inform postoperative surveillance regimens.4 For example, prevention strategies may include use of prophylactic antibiotics, reducing operative duration, aggressively treating preoperative urinary tract infections, and using caution in elderly patients or patients with a higher Charlson comorbidity index.8 If urosepsis does occur, postoperative treatment options may include drainage of the urinary tract and culture-specific antibiotic therapy.5 In addition to the preoperative risk factors, we speculate that the technical specifications of the available URS instruments (i.e., reusable versus disposable instruments, instruments that can facilitate better control of intrarenal pressure, etc.) may also have an impact on the risk of urosepsis. In an observational study by Qiang and colleagues (2016) on the clinical features of urosepsis in critical care medicine, the authors discuss that increases in intrarenal pressure may allow bacteria to enter the bloodstream and induce bacteremia.9 To manage this risk, the authors suggest reducing intrarenal pressure peaks during the operation and reducing the hypoperfusion pressure.9
In summary, many urologists may not be aware of the high incidence rate of urosepsis after URS. To mitigate the impact of this complication, urologists performing URS should be aware of the factors that increase urosepsis risk, the strategies for preventing urosepsis in the preoperative setting, the need for postoperative surveillance of high-risk patients, the available treatment options if urosepsis does occur, and conceivably the technical characteristics and specifications of the available instruments for performing URS.
Written by: Naeem Bhojani, MD,1 Ben Cutone, MPH, MSc,2 & Ben H. Chew, MD3
- Division of Urology, Centre Hospitalier de l’Universite´ de Montréal, Montréal, Canada
- Health Economics and Market Access, Boston Scientific, Marlborough, Massachusetts, USA
- Department of Urologic Sciences, University of British Columbia, Vancouver, Canada
The study discussed within this article was supported by Boston Scientific. Dr. Bhojani and Dr. Chew report a consultancy with Boston Scientific. Dr. Bhojani and Dr. Chew were not compensated for the study nor for this Beyond the Abstract article. Mr. Cutone is employed by Boston Scientific. Author disclosure:
Disclaimer: The views and opinions expressed in this Editorial are those of the authors and do not necessarily reflect the official policy or position of Boston Scientific.
References:
- Chewcharat A, Curhan G. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis. 2021;49(1):27-39. doi:10.1007/s00240-020-01210-w
- Abufaraj M, Xu T, Cao C, et al. Prevalence and Trends in Kidney Stone Among Adults in the USA: Analyses of National Health and Nutrition Examination Survey 2007-2018 Data [published online ahead of print, 2020 Sep 5]. Eur Urol Focus. 2020;S2405-4569(20)30224-8. doi:10.1016/j.euf.2020.08.011.
- Scales CD Jr, Smith AC, Hanley JM, Saigal CS; Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160-165. doi:10.1016/j.eururo.2012.03.052
- Bhojani N, Miller LE, Bhattacharyya S, Cutone B, Chew BH. Risk Factors for Urosepsis After URS for Stone Disease: A Systematic Review with Meta-Analysis [published online ahead of print, 2021 Mar 15]. J Endourol. 2021;10.1089/end.2020.1133. doi:10.1089/end.2020.1133
- De Coninck V, Keller EX, Somani B, et al. Complications of URS: a complete overview. World J Urol. 2020;38(9):2147-2166. doi:10.1007/s00345-019-03012-1.
- Geraghty RM, Jones P, Somani BK. Worldwide Trends of Urinary Stone Disease Treatment Over the Last Two Decades: A Systematic Review. J Endourol. 2017;31(6):547-556. doi:10.1089/end.2016.0895
- Porat A, Bhutta BS, Kesler S. Urosepsis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 7, 2021.
- Chugh S, Pietropaolo A, Montanari E, Sarica K, Somani BK. Predictors of Urinary Infections and Urosepsis After URS for Stone Disease: a Systematic Review from EAU Section of Urolithiasis (EULIS). Curr Urol Rep. 2020;21(4):16. Published 2020 Mar 24. doi:10.1007/s11934-020-0969-2
- Qiang XH, Yu TO, Li YN, Zhou LX. Prognosis Risk of Urosepsis in Critical Care Medicine: A Prospective Observational Study. Biomed Res Int. 2016;2016:9028924. doi:10.1155/2016/9028924
Read the Abstract


