BERKELEY, CA (UroToday.com) - In our recently published article “A Nephrolithometric Nomogram To Predict Treatment Success of Percutaneous Nephrolithotomy," we present a nomogram to predict treatment success of patients with kidney stones. Historically, nomograms are widely used in oncological fields, and predictive tools for non-life threatening diseases were not available. Recently, there has been a growing interest in developing nomograms for non-life threatening diseases, such as kidney stones.[1] We developed a nomogram for patients presenting with this common benign medical condition, because, until now, there was no reliable prognostic tool that could be used to optimize treatment for patients suffering from kidney stones.
This study was coordinated by the Clinical Research Office of the Endourological Society (CROES), which offers a global platform to conduct endourological research. The CROES Percutaneous Nephrolithotomy (PNL) Global Study was set up to gain a better understanding of indications, outcomes, and risk factors for this treatment. Including 5 803 patients from over 90 centers worldwide, it gives an unprecedented insight into a variety of research questions considering PNL. This study is described in detail elsewhere,[2] and has already been the source of more than 25 articles that have been published.
Rather than delving into the methodological issues we were confronted with during this study, we would like to share with you our view of the implications of this nomogram for everyday clinical use.
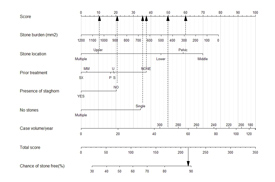 To appreciate the implications of this tool, we will briefly outline the patient population it is intended for and the variables it relies on. Our nomogram is developed for patients with kidney stones who are planned to undergo percutaneous nephrolithotomy. It predicts treatment success in those patients based on 6 parameters (see Figure). These mostly radiological parameters are commonly assessed, and include stone burden, location, presence of staghorn, number of stones, and also prior treatment and annual case volume of the center. Five of these parameters are patient-specific, so treatment success is largely dependent on the condition of the patient who will undergo PNL. However, there is one center-specific parameter, annual case volume, that has a great influence, too.
To appreciate the implications of this tool, we will briefly outline the patient population it is intended for and the variables it relies on. Our nomogram is developed for patients with kidney stones who are planned to undergo percutaneous nephrolithotomy. It predicts treatment success in those patients based on 6 parameters (see Figure). These mostly radiological parameters are commonly assessed, and include stone burden, location, presence of staghorn, number of stones, and also prior treatment and annual case volume of the center. Five of these parameters are patient-specific, so treatment success is largely dependent on the condition of the patient who will undergo PNL. However, there is one center-specific parameter, annual case volume, that has a great influence, too.
This center-specific parameter shows two important features of the nomogram. First, it shows that patient-specific factors are not the only factors that influence treatment outcomes. Although it was already known that factors, other than the condition of the patient, are associated with treatment success,[3] it is once more established by this predictive tool. This realisation can be very useful for both the patient and the clinician in discussing treatment success and outcomes. Second, it shows that it will not be appropriate to develop one standard, universal predictive nomogram for all patients who will undergo PNL, since center-specific factors are not always measured or even known. Rather, this nomogram could be guidance to urologists and should inspire them to fine-tune this nomogram at center-specific directions.
Not only case volume differs between centers, but also surgeon experience varies within these centers. It is safe to assume that surgeon experience is also largely influential on stone-free status after PNL.[4] So the final result of the PNL is not only dependent on the factors that are included in this nomogram, but also on surgeon skills, available tools at OR, or other factors that are not easily measured and are variable between centers. Therefore, we advise clinicians to try and improve this nomogram, based on local information collected in their center.
In the meantime, this nomogram is a strong predictive tool to be used in anticipation management for the patient as well as for the clinician. In calculating the stone-free chance after PNL, urologists can provide themselves with additional information on the procedure. Patients’ anticipation can be managed by showing the chances of becoming stone free after surgery. Especially when this calculated chance is low, it provides clinicians with a visual tool to gain better understanding in patients. This way, the patient-clinician relationship will hopefully benefit, which results in better treatment of these patients.
References:
- Kanao K, Nakashima J, Nakagawa K, et al. Preoperative nomograms for predicting stone-free rate after extracorporeal shock wave lithotripsy. J Urol 2006;176(4 Pt 1):1453–6; discussion 1456–7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16952658. Accessed June 25, 2013.
- De la Rosette JJMCH, Assimos D, Desai M, et al. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study : Journal of Endourology / Endourological Society. 2011;25(1):11–17.
- Turk C, Knoll T, Petrik A, et al. Guidelines on Urolithiasis. 2013;40(4). Available at: http://www.uroweb.org/gls/pdf/21_Urolithiasis_LR.pdf.
- Opondo D, Tefekli A, Esen T, et al. Impact of case volumes on the outcomes of percutaneous nephrolithotomy. European Urology. 2012;62(6):1181–7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/22440402. Accessed July 2, 2013.
Written by:
Jean J.M.C.H. de la Rosette, MD, PhD as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.
Academic Medical Center, University of Amsterdam, Department of Urology, Amsterdam, The Netherlands
A nephrolithometric nomogram for predicting treatment success in percutaneous nephrolithotomy - Abstract

More Information about Beyond the Abstract


