Transurethral resection of the prostate (TURP) is the gold standard surgical treatment, but this and less-invasive techniques that involve tissue destruction are associated with substantial comorbidities, whereas prostatic urethral lift (PUL) is minimally invasive (Figure 1)
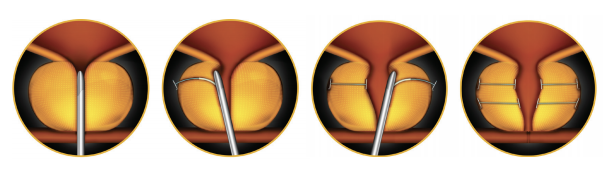
Figure 1. Placement of PUL implants to retract obstructive prostate lobes without tissue-destructive procedures
Tissue effects of different prostate-reduction techniques versus prostatic urethral lift. Transurethral resection of the prostate (TURP) has been the surgical gold standard since the 1970s, and improves subjective symptoms and urinary flow, but is associated with significant morbidity and long-term complications such as urinary incontinence, strictures, infections, and sexual dysfunction. Laser-based techniques are associated with less bleeding and hospitalization, but these still work by tissue removal or destruction, leading to similar perioperative complications and the same list of permanent complications as TURP2,3 . Prostatic urethral lift is a minimally invasive technique that moves the prostate lobes apart, obviating effects associated with tissue destructive procedures. We compared whether treatment of BPH with PUL would improve treatment-related outcomes and costs compared with monopolar or bipolar TURP.
Methods: We were provided with derived outputs by Harvey Walsh Ltd who have licensed access to the National Health Service Hospital Episode Statistics (HES) database (Copyright NHS Digital 2018) and The Health Improvement Network (THIN) to search at the record level for hospitalization and treatment rates for TURP in England. The HES database holds information (ICD10 codes) on all admissions, accident and emergency visits and outpatient appointments at NHS hospitals in England. The THIN database includes information (ICD10 and Read codes) on diagnoses, treatments, care, and visits for patients in primary care from more than 400 general practice surgeries in the UK. To compare complications, we searched HES and THIN for each recording of 25 ICD10 codes (Table 1) that could reasonably be assumed to be directly related to non-laser TURP (procedural classifications M651 and M653) in all men who underwent this surgery for BPH in England in 2009/10, and drew on data from the literature for further information on those that were most common.
We calculated the potential annual difference in operative and postoperative costs between TURP and PUL based on the most common complication and re-treatment rates4–10 and assuming 50% uptake for PUL.

Results: TURP - In 2016/17, 18,362 monopolar and bipolar TURP procedures were reported in HES. The average hospital stay is 2.7 days, and catheterization is required for 3–5 days on average. Although rates vary, complications of TURP include ejaculatory dysfunction, affecting at least 65% men,7 erectile dysfunctions in ~10%,7 urethral stricture in ~4%, infection in ~4%, bleeding requiring transfusion in ~2%, and permanent urinary incontinence in ~2%. 1–2% of patients require TURP reoperation per year8 but around 14% of patients restart drug therapy for LUTS within 12 months, around 20% by 3 years, and around 40% by 5 years10 . Among all recipients of TURP for BPH in 2009/10, cumulative HES data to 2014/15 showed 70,000 post-procedure hospital spells PUL . The longest-term data reported for PUL are 5-year outcomes and compare the procedure with sham surgery11 . No hospital stays were required and catheterization, required for 32%, was 1 day on average. Most adverse events (mainly dysuria, discomfort, urgency, and haematuria) were mild to moderate and most resolved in 2–4 weeks without hospital treatment. Erectile and ejaculatory function were preserved with no incident cases of sustained dysfunction reported after surgery. The surgical re-treatment rate was 13.6% (4.3% repeat PUL, 9.3% TURP or laser ablation), but all but one of the re-treated patients had severe to very severe LUTS at baseline. Medical treatment was restarted in just under 4% of patients at 1 year and in 11% of patients 5 years after surgery. Based on this complication profile, we estimate that the complication rate associated with TURP could be halved with PUL and, therefore, that a saving of £27 million could be made per year.
Cost calculations and estimated saving with PUL versus TURP. TURP Mean 2016/17 procedure cost for TURP (national schedule of reference costs) £2,869 (IQR £2,422–3,138), giving a minimum total of ~£43 million. Complications cost to payer £109 million over 5 years for each annual cohort of patients PUL. Mean 2015/16 cost for PUL (calculated by The National Institute for Health and Care Excellence) £2,40512. Assumptions: – Rate of described complications reduced by 50% – Uptake of PUL would be 50% ESTIMATED SAVING £27 million per year over 5 years for each annual cohort of patients.
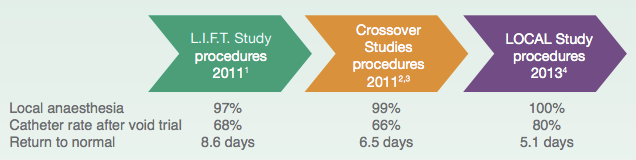
Conclusions: Durability of the treatment is similar for TURP and PUL, but the postoperative complication and medical re-treatment profiles differ. PUL is associated with a very low rate of complications, most of which are mild to moderate in severity and resolve within 2–4 weeks. Increasing experience with PUL procedures, which is associated with increased numbers of procedures performed under local anesthetic and rapidity of recovery, is likely to improve outcomes further (Figure 2)13–15. For a similar procedural cost, PUL could reduce complications, improve quality of life, and substantially reduce post-surgical care costs compared with current standard TURP practice.
References:
Jung JH, McCutcheon KA, Reddy B, et al. Prostatic urethral lift for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia (protocol). Cochrane Syst Rev Database 2017; 10: CD012832.
2. Li S, Zeng X-T, Ruan X-L, et al. Holmium laser enucleation versus transurethral resection in patients with benign prostate hyperplasia: an updated systematic review with meta-analysis and trial sequential analysis. PLoS One 2014; 9: e101615.
3. Naspro R, Bachmann A, Gilling P, et al. A review of the recent evidence (2006–2008) for 532-nm photoselective laser vaporisation and holmium laser enucleation of the prostate. Eur Urol 2009; 55: 1345–57.
4. McNicholas TA. Benign prostatic hyperplasia and new treatment options – a critical appraisal of the UroLift system. Med Devices (Auckl) 2016; 9: 115–23.
5. Lourenco T, Armstrong N, N’Dow J, et al. Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement. London: HMSO, 2008.
6. Ray A, Morgan H, Carolan-Rees G. External assessment centre report: the Urolift system for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. Cardiff: Cedar, 2015.
7. American Urological Association. Chapter 1: AUA guideline on the management and treatment of benign prostatic hyperplasia: diagnosis and treatment recommendations. Linthicum, MD: American Urological Association Education and Research Inc, 2003.
8. American Urological Association. Chapter 1: AUA guideline on the management and treatment of benign prostatic hyperplasia (BPH). Linthicum, MD: American Urological Association Education and Research Inc, 2010.
9. Miano R, De Nunzio C, Asimakopoulos AD, et al. Treatment options for benign prostatic hyperplasia in older men. Med Sci Monit 2008; 14: RA94–102.
10. Lukacs B, Cornu J-N, Aout M, et al. Management of lower urinary tract symptoms relation to benign prostatic hyperplasia in real-life practice in France: a comprehensive population study. Eur Urol 2013; 64: 493–501.
11. Roehrborn CG, Barkin J, Gange SN, et al. Five year results of the prospective randomized control prostatic urethral L.I.F.T. study. Can J Urol 2017; 24: 8802–13.
12. NICE. Costing statement: UroLift for treating lower urinary tract symptoms of benign prostatic hyperplasia (MTG26). London: National Institute for Health and Care Excellence, 2015. 13. Cantwell AL, Bogache WK, Richardson SF, et al. Multicentre prospective crossover study of the ‘prostatic urethral lift’ for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. BJU Int 2014; 113: 615–22. 14. Rukstalis D, Rashid P, Bogache WK, et al. 24-month durability after crossover to the prostatic urethral lift from randomised, blinded sham. BJU Int 2016; 118 (suppl 3): 14–22. 15. Shore N, Freedman S, Gange S, et al. Prospective multi-center study elucidating patient experience after prostatic urethral lift. Can J Urol 2014; 21: 7094–101.
Authors: Orlowski A1 , Wilkins J1 , Kayes O2
Author Information:
1.Imperial College Health Partners, London, United Kingdom
2.Leeds Teaching Hospitals Trust, Leeds, United Kingdom


