In our study, we leveraged American Board of Urology (ABU) case log data from over 6,500 U.S. urologists who performed nearly 74,000 surgeries for BPH between 2008-2021 to assess evolving practice patterns. While prior ABU case log studies demonstrated its utility as a unique resource to assess surgeon demographics and practice pattern variation, our study provides contemporary findings after the CPT codification of two innovative, major BPH surgical technologies: holmium laser enucleation of the prostate (HoLEP) in 2007 and prostatic urethral lift (PUL) in 2015.
While we hypothesized that the use of transurethral resection of the prostate (TURP)—the historic gold standard surgical treatment for BPH—decreased significantly over time, our results suggest otherwise. Despite the advent of multiple competing surgical techniques, traditional TURP remained dominant during our study period, comprising approximately half of BPH surgeries (Figure). In fact, TURP remained the most common BPH surgical approach annually except 2011, when photoselective vaporization of the prostate (PVP) was most prevalent. Furthermore, in adjusted analyses, the odds of performing TURP actually increased year-over-year.
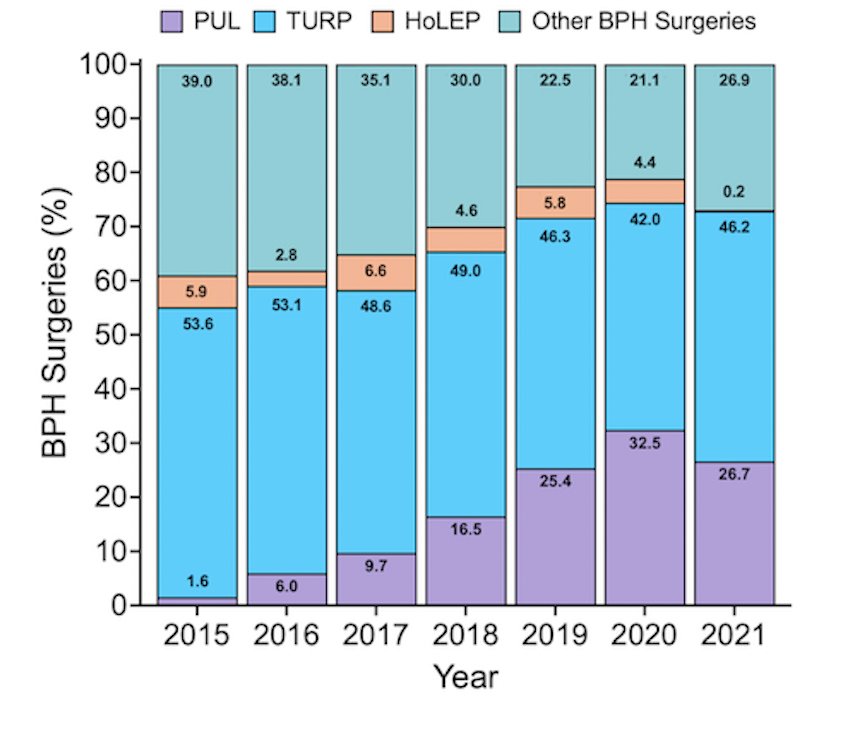
Figure: Temporal variation in benign prostatic hyperplasia surgical modalities
Notably, the fastest growing modality was PUL, which increased from 1.6 to 32.5% of BPH surgeries from 2015 to 2020. In adjusted analyses, factors associated with performing PUL included higher BPH surgeon volume and subspecialization in andrology, the latter of which may be related to an increased interest in preserving ejaculatory function via PUL. Others have also reported the significant growth of PUL utilization, which may be attributable to its easier learning curve, higher reimbursement on a per-implant basis, and aid from industry-led marketing.
In contrast, HoLEP experienced no significant growth since its introduction, comprising just 3-6% of BPH surgeries annually, despite multiple randomized controlled trials showing equivalent or improved outcomes compared to TURP and an equivalent grade B recommendation from the AUA. Academic and higher-volume urologists were more likely to perform HoLEP. Potential barriers to adoption include a challenging learning curve, geographic and practice-based gaps in equipment availability, and lack of industry backing.
Overall, we demonstrate the staying power of TURP, which remains the most commonly performed BPH surgery in the United States. Although PUL is a grade C recommendation only indicated for men with prostate volume 30-80 cc and documented absence of obstructing median lobe, it was rapidly adopted in contrast to HoLEP, despite high-level evidence and a prostate volume-independent grade B recommendation. Given the numerous existing techniques available to providers and patients and generally broad guidelines, it seems likely that practice variation will continue to exist in this space, highlighting the importance of shared decision making between patients and providers.
Read the Abstract


