Thus, the objective of our study was to investigate the feasibility and safety of performing WVTT without postoperative catheterization among men with BPH. The study design is summarized in Figure 1.
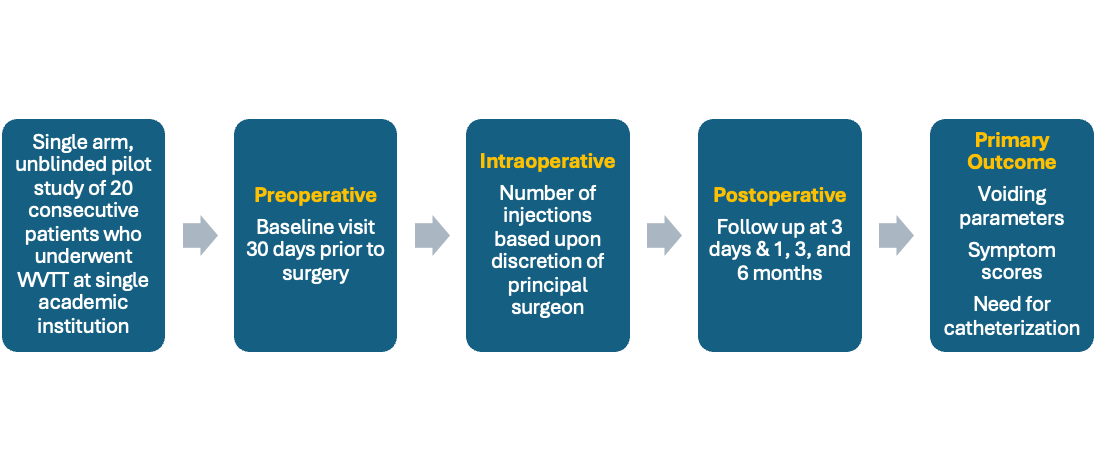
Figure 1. Catheter-free WVTT pilot study design.
We included patients ages 40-80 with prostate size 30-80cc by transrectal ultrasound (TRUS), maximum flow rate (Qmax) <15ml/s. All patients underwent preoperative urodynamics and had a bladder contractility index (BCI) >100 to rule out detrusor underactivity or atonic bladder. We excluded patients with preoperative catheterization or post-void residual >400ml.
The mean age of the cohort was 65 years (range: 55-75). The mean prostate size was 43cc (range: 30-68). 30% (n=6) of patients had a median lobe; these patients underwent 3 injections, whereas the remaining 14 (70%) underwent 2 injections. Every patient underwent WVTT under local anesthesia in the outpatient setting.
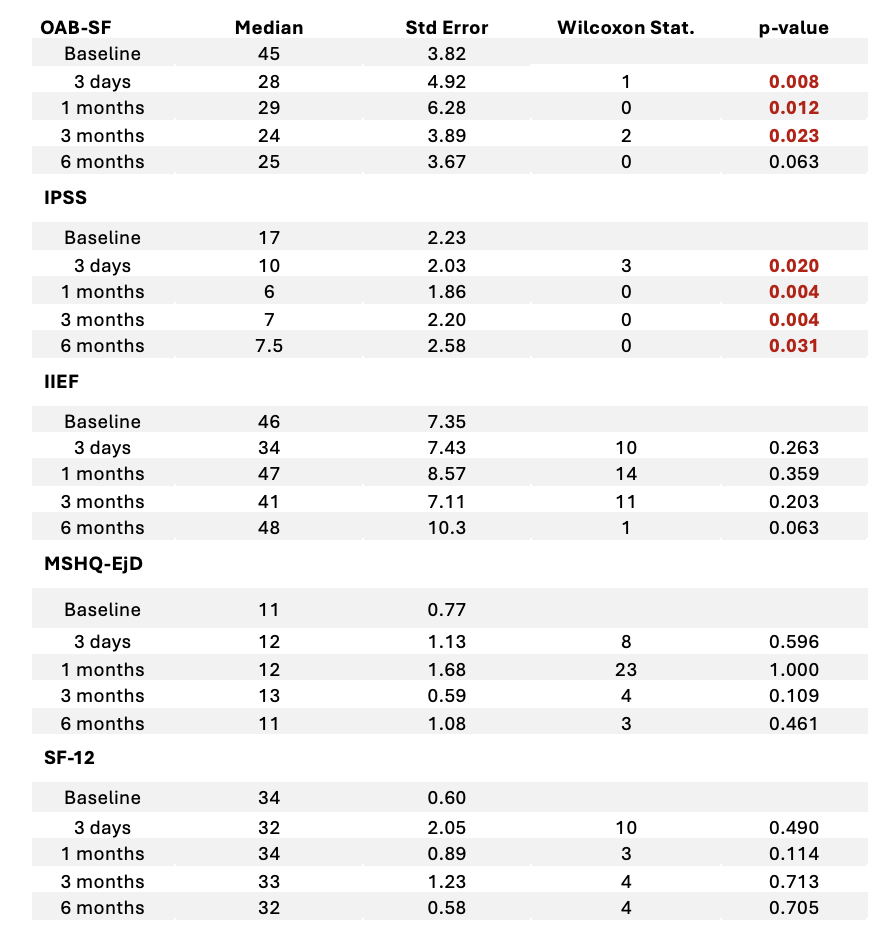
One patient (5%) required catheterization on postoperative day 2 for acute urinary retention. No patients required antibiotics for postoperative infection or readmission within 30 days. There were significant increases in voided volume and Qmax (p<0.05; Table 1). There were also significant improvements in symptom scores including the International Prostate Symptom Score (IPSS) and the Overactive Bladder Short Form (OAB-SF; p<0.05; Table 2) without significant change in sexual function.
Table 1. Voiding parameters compared between baseline and postoperative follow-up at 3 days, 1 month, 3 months, and 6 months.
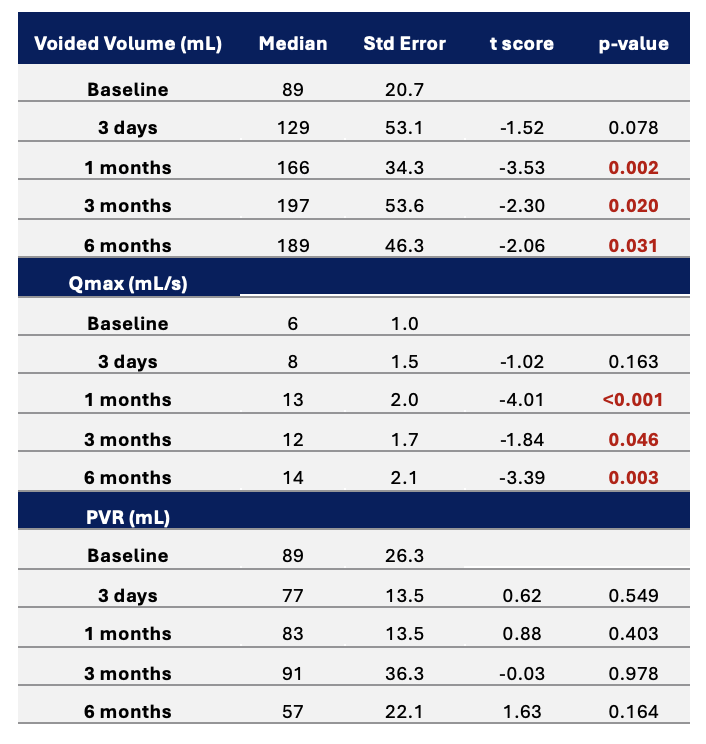
Table 2. Symptom scores compared between baseline and postoperative follow-up at 3 days, 1 month, 3 months, and 6 months.
We acknowledge our study was limited by its small sample size and lack of control arm. We also recognize our patients were well-selected with small prostate volume, low PVR, and lack of detrusor underactivity. Our hope is this pilot study will serve as the foundation for a larger, robust multi-institutional study evaluating outcomes of catheter-free WVTT.
Key Takeaways
- Catheter-free WVTT resulted in improved voiding parameters and symptom scores
- No changes in sexual function, infectious complications, or readmissions noted
- Only 1 patient (5% rate) required postoperative catheterization within the first 30 days
- Catheter-free WVTT is feasible in well-selected patients and larger studies with longer follow up are needed
- UC San Diego Health, San Diego, CA, USA
- Weill Cornell Medicine, New York, NY, USA
- University of Montreal Hospital Center (CHUM), Montreal, QC, Canada
- BPH Canada Prostate Center, Montreal, QC, Canada
- University Health Network, University of Toronto, Toronto, ON, Canada
- Northwell Health, New Hyde Park, NY, USA
- Lerner LB, McVary KT, Barry MJ, et al. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA GUIDELINE PART I-Initial Workup and Medical Management. J Urol. 2021;206(4):806-817.
- McVary KT, Gange SN, Gittelman MC, et al. Erectile and Ejaculatory Function Preserved With Convective Water Vapor Energy Treatment of Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia: Randomized Controlled Study. J Sex Med. 2016;13(6):924-933.
- McVary KT, Rogers T, Roehrborn CG. Rezūm Water Vapor Thermal Therapy for Lower Urinary Tract Symptoms Associated With Benign Prostatic Hyperplasia: 4-Year Results From Randomized Controlled Study. Urology. 2019;126:171-179.


