Concurrently, physicians are often not aware of the out-of-pocket (OOP) expenses of the medical treatments and procedures that they provide to their patients.4,5 Furthermore, the American Urological Association (AUA) 2018 guidelines on ED do not include a discussion of the costs of available treatment options.6
Thus, we devised a Medicare cost model to estimate patient OOP costs for the six AUA guideline-recommended ED treatments,7 as outlined in Table 1.
Table 1" 2018 AUA guideline recommendations for treatment of ED.

Coverage policies were obtained from the Medicare Coverage Database and OOP cost was retrieved from the 2023 Centers for Medicare and Medicaid Services Final Rule. OOP cost for treatments without Medicare coverage were extracted from GoodRx or literature and inflated to 2022 dollars. Annual prescription costs were calculated using the published estimate of 52.2 yearly instances of sexual intercourse among men aged 57 to 72 years in the United States.8 An annual IA prescription had the highest OOP cost ($4022), followed by an annual ICI prescription ($3947), one ESWT treatment course ($3445), IPP as an outpatient procedure ($1600), annual PDE5i prescription ($696), and one VED unit ($213; Figure 1). Among PDE5i medications, avanafil is associated with the highest annual cost ($3455), followed by vardenafil ($2102), tadalafil ($723), and sildenafil ($459).
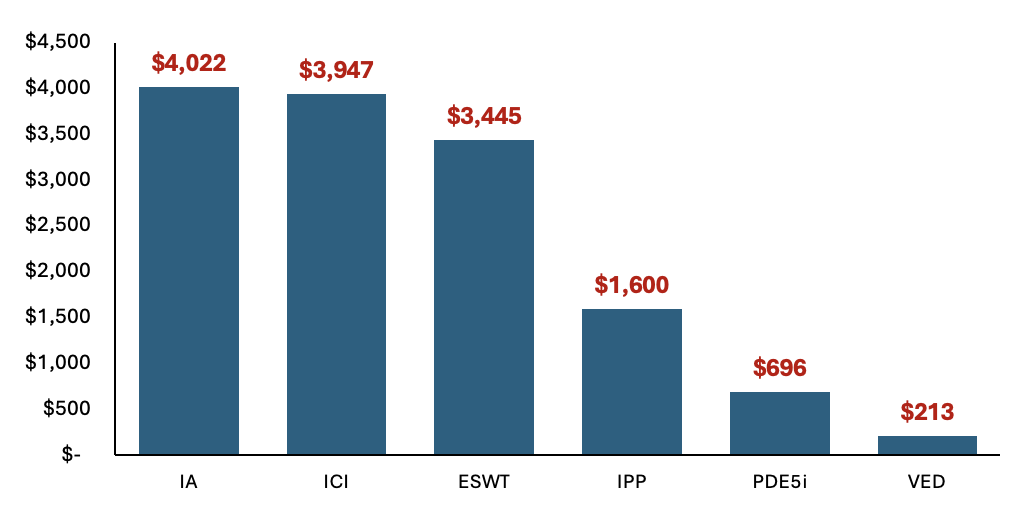
Figure 1. Annual patient out-of-pocket costs for guideline-recommended ED treatments.
To understand the potential US healthcare system economic implications, this model referenced the estimated number of men age 65 and older with moderate-to-severe ED covered by Medicare (n=254,650)9. IA is associated with the highest cumulative national healthcare OOP costs ($1.02 billion annually), followed by ICI ($1.0 billion), ESWT ($877 million), IPP ($407 million), PDE5i ($177 million), and VED ($54 million).
There were limitations to our model, which include the abstraction of data from several sources, the conservative assumption that each patient would only trial one treatment option annually, and the lack of generalizability of our findings to patients not covered by Medicare.
Future areas of study include the incorporation of online prescription platforms and direct-to-consumer (DTC) care. Factors that likely contribute to the rising popularity of this care model include both time and geographic convenience. In addition, as mentioned above, patients who perceive their medical problems to be shameful, such as men with ED, may prefer this service as it bypasses in-person interaction with a provider.10 Given the wide variety of these services, it remains unknown the range of costs of prescriptions obtained online.11
Prior studies have highlighted the potential cost savings to be garnered from urologic drug price stewardship.12 Cortese et al. demonstrated a potential savings of approximately $1.29 billion in 2020 if Medicare prices for generic urologic drugs were as low as those offered by the Mark Cuban Cost Plus Drug Company, a public benefit corporation centered on manufacturing and distribution of lower-priced generic drugs.12 Thus, we hope that our findings will, in fact, change the clinical management of ED by increasing awareness into the cost variation among the different guideline-recommended treatments.
In sum, we have highlighted our key takeaways as below. We hope that our model will encourage providers to not only consider individual patient financial burden but also cost-effectiveness from a broader high-value care lens to ultimately improve shared decision-making with patients who suffer from ED.
Key Takeaways:
- U.S. healthcare costs rank among the highest in the world
- Many physicians have limited insight into the costs and insurance coverage of the treatment options that they recommend
- This is the first study to develop a Medicare-based cost model estimating OOP costs for patients seeking ED treatments
- The AUA 2018 ED guidelines do not discuss cost of recommended treatment options
- Oral PDE5i and IPP are cost-effective options with strong AUA guideline recommendations
UC San Diego Health, San Diego, CA, USA
References:
- Lyngdorf P, Hemmingsen L. Epidemiology of erectile dysfunction and its risk factors: a practice-based study in Denmark. Int J Impot Res. 2004;16(2):105-111.
- Kubin M, Wagner G, Fugl-Meyer AR. Epidemiology of erectile dysfunction. Int J Impot Res. 2003;15(1):63-71. doi:10.1038/sj.ijir.3900949
- Shabsigh R, Perelman MA, Laumann EO, Lockhart DC. Drivers and barriers to seeking treatment for erectile dysfunction: a comparison of six countries. BJU Int. 2004;94(7):1055-1065.
- Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283.
- Schutte T, Tichelaar J, Nanayakkara P, Richir M, van Agtmael M. Students and Doctors are Unaware of the Cost of Drugs they Frequently Prescribe. Basic Clin Pharmacol Toxicol. 2017;120(3):278-283.
- Burnett AL, Nehra A, Breau RH, et al. Erectile Dysfunction: AUA Guideline. J Urol. 2018;200(3):633-641.
- Nguyen V, McGovern AM, Rojanasarot S, et al. Patient out-of-pocket costs for guideline-recommended treatments for erectile dysfunction: a medicare cost modeling analysis. Int J Impot Res. Published online June 26, 2024.
- Karraker A, Delamater J, Schwartz CR. Sexual frequency decline from midlife to later life. J Gerontol B Psychol Sci Soc Sci. 2011;66(4):502-512.
- Rojanasarot S, Williams AO, Edwards N, Khera M. Quantifying the number of US men with erectile dysfunction who are potential candidates for penile prosthesis implantation. Sex Med. 2023;11(2):qfad010.
- Rodler S, von Büren J, Buchner A, et al. Epidemiology and Treatment Barriers of Patients With Erectile Dysfunction Using an Online Prescription Platform: A Cross-Sectional Study. Sex Med. 2020;8(3):370-377.
- Dietrich PN, Doolittle J, Brink S, et al. An Online Investigation Into Direct-to-Consumer Men’s Health Clinics: The Who, What, and Where. Urology. 2023;174:135-140. doi:10.1016/j.urology.2023.01.026
- Cortese BD, Chang SS, Talwar R. Urological Drug Price Stewardship: Potential Cost Savings Based on the Mark Cuban Cost Plus Drug Company Model. Journal of Urology. 2023;209(2):309-311.


