RIO DE JANEIRO, BRAZIL (UroToday.com) - Presented by Michael Kennelly,1 Heinrich Schulte-Baukloh,2 Roger Dmochowski,3 Karen Ethans,4 Courtenay Moore,5 Yan Zheng,6 Steven Guard,7 Brenda Jenkins,8 and Gilles Karsenty9 at the International Continence Society (ICS) 2014 Annual Meeting - October 20 - 24, 2014 - Rio de Janeiro, Brazil
ABSTRACT:
Hypothesis/Aims of Study
Patients with spinal cord injury (SCI) often have neurogenic detrusor overactivity (NDO), which frequently results in urinary incontinence (UI) and elevated intravesical pressures that may impair patients’ quality of life (QOL) and increase their risk for the development of renal dysfunction. OnabotulinumtoxinA (BOTOX®; Allergan, Inc) has been shown to be well tolerated and effective in the treatment of NDO due to SCI or multiple sclerosis (MS) in two phase 3, randomized, placebo-controlled, double-blind studies in patients who are not adequately managed by at least 1 anticholinergic. A large, long-term, multicenter, extension study of onabotulinumtoxinA, in which patients were eligible to receive multiple treatments for a total of up to 4 years, has also been conducted. Here we present the final results of the long-term efficacy and safety of onabotulinumtoxinA in the cohort of patients with SCI.
Study Design, Materials and Methods
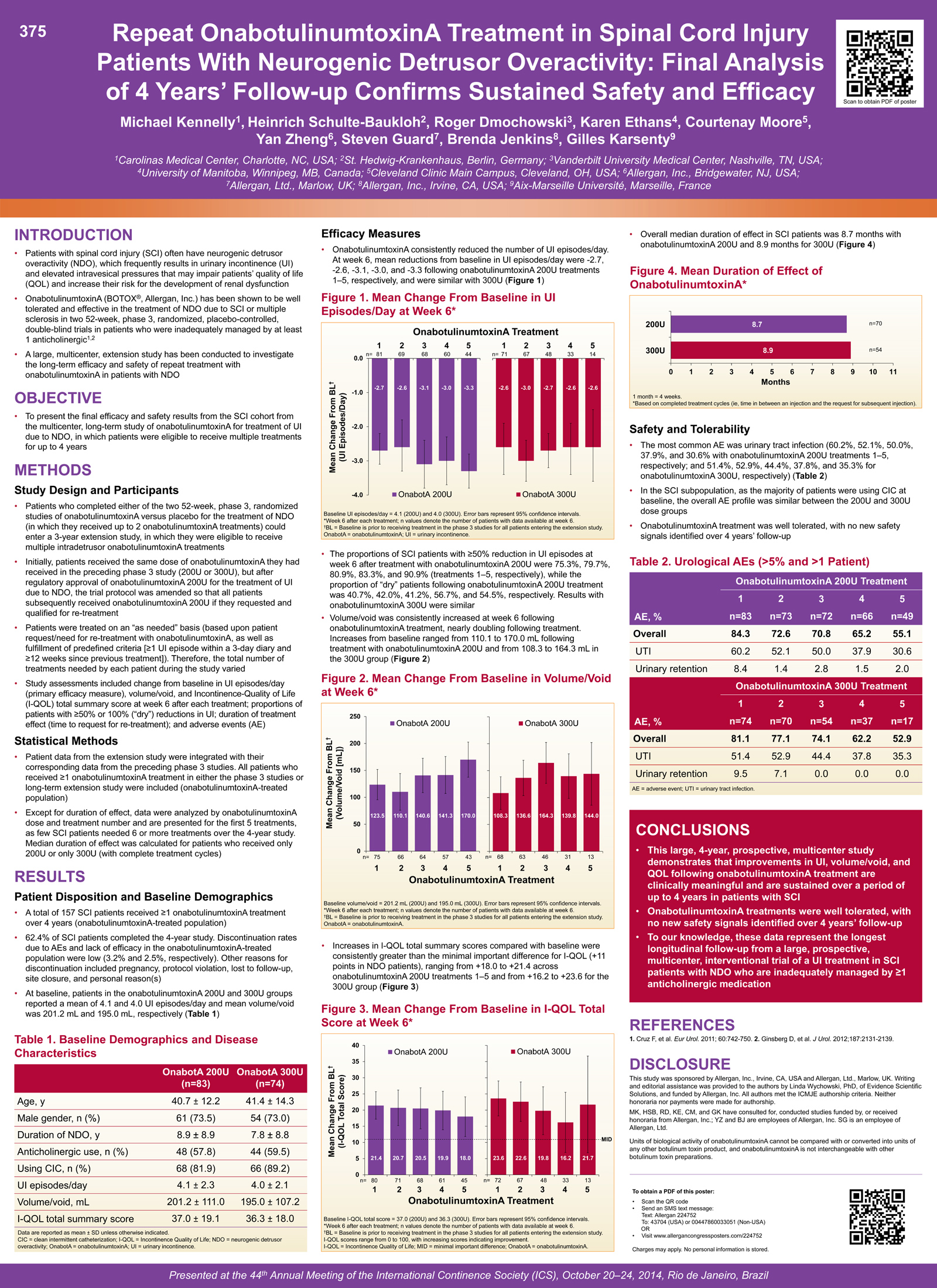 Patients who completed either of the two 52-week, phase 3, randomized studies of onabotulinumtoxinA for the treatment of NDO due to SCI or MS (in which they received up to 2 onabotulinumtoxinA treatments) could enter a 3-year extension study in which they received multiple intradetrusor onabotulinumtoxinA treatments. Initially patients received the same dose of onabotulinumtoxinA they had received in the preceding phase 3 study (200U or 300U), but after regulatory approval of onabotulinumtoxinA 200U for the treatment of UI due to NDO, the trial protocol was amended so that all patients subsequently received onabotulinumtoxinA 200U (if they requested and qualified for retreatment). Treatment schedules were individualized and were based upon patient request/need for retreatment as well as a predefined threshold of ≥ 1 UI episode within a 3-day diary and at least 12 weeks since previous onabotulinumtoxinA treatment. Study assessments included change from baseline in UI episodes/day (primary efficacy measure), volume/void, and Incontinence-Quality of Life (I-QOL) total summary score at week 6 after each treatment; proportions of patients with ≥ 50% or 100% (‘dry’) reductions in UI; duration of treatment effect (time to request for retreatment); and adverse events (AEs). Data are presented by onabotulinumtoxinA treatment cycle (i.e., the 1st, 2nd, 3rd, etc, onabotulinumtoxinA treatment received); duration data are presented as overall median duration of effect for all SCI patients with complete treatment cycles. Data are presented for the first 5 treatment cycles, as few SCI patients received 6 or more treatments over the 4-year study.
Patients who completed either of the two 52-week, phase 3, randomized studies of onabotulinumtoxinA for the treatment of NDO due to SCI or MS (in which they received up to 2 onabotulinumtoxinA treatments) could enter a 3-year extension study in which they received multiple intradetrusor onabotulinumtoxinA treatments. Initially patients received the same dose of onabotulinumtoxinA they had received in the preceding phase 3 study (200U or 300U), but after regulatory approval of onabotulinumtoxinA 200U for the treatment of UI due to NDO, the trial protocol was amended so that all patients subsequently received onabotulinumtoxinA 200U (if they requested and qualified for retreatment). Treatment schedules were individualized and were based upon patient request/need for retreatment as well as a predefined threshold of ≥ 1 UI episode within a 3-day diary and at least 12 weeks since previous onabotulinumtoxinA treatment. Study assessments included change from baseline in UI episodes/day (primary efficacy measure), volume/void, and Incontinence-Quality of Life (I-QOL) total summary score at week 6 after each treatment; proportions of patients with ≥ 50% or 100% (‘dry’) reductions in UI; duration of treatment effect (time to request for retreatment); and adverse events (AEs). Data are presented by onabotulinumtoxinA treatment cycle (i.e., the 1st, 2nd, 3rd, etc, onabotulinumtoxinA treatment received); duration data are presented as overall median duration of effect for all SCI patients with complete treatment cycles. Data are presented for the first 5 treatment cycles, as few SCI patients received 6 or more treatments over the 4-year study.
Results
A total of 157 SCI patients entered the long-term study and received at least 1 onabotulinumtoxinA treatment over 4 years. Retreatment schedules were individualized per protocol (based on the patient’s request and the investigator’s assessment of prespecified retreatment criteria), so the number of treatments each patient received during their participation in the study varied. At study baseline, SCI patients reported an average of 4.1 UI episodes/day and volume/void was 201.2 mL. Repeat onabotulinumtoxinA treatment consistently reduced the number of UI episodes/day; mean changes from baseline in UI episodes/day at week 6 following onabotulinumtoxinA 200U treatment were -2.7, -2.6, -3.1, -3.0, and -3.3 (cycles 1-5, respectively). The proportions of SCI patients with ≥ 50% reduction in UI episodes at week 6 after treatment with onabotulinumtoxinA 200U were 75.3%, 79.7%, 80.9%, 83.3%, and 90.9% (cycles 1-5, respectively), while the proportion of ‘dry’ patients following onabotulinumtoxinA 200U treatment was 40.7%, 42.0%, 41.2%, 56.7% and 54.5%, respectively. Volume/void consistently increased after each onabotulinumtoxinA treatment, with increases from baseline at week 6 ranging from 110.1 to 170.0 mL. Increases in I-QOL total summary scores compared to baseline were consistently greater than the minimally important difference for I-QOL (+11 points in NDO patients), ranging from +18.0 to +21.4 across onabotulinumtoxinA 200U treatment cycles 1-5. Overall median duration of effect (time to request for retreatment) for onabotulinumtoxinA 200U in SCI patients with complete treatment cycles was 34.7 weeks. Efficacy results for onabotulinumtoxinA 300U (which some patients received before the protocol amendment) were similar. Discontinuation rates due to AEs and lack of efficacy were low at 3.2% and 2.5%, respectively; the overall discontinuation rate was 37.6% over 4 years. Other reasons for discontinuation included pregnancy, protocol violation, lost to follow-up, site closure, and personal reason. The most common AE observed was urinary tract infection (60.2%, 52.1%, 50.0%, 37.9% and 30.6% with onabotulinumtoxinA 200U in treatment cycles 1-5, respectively). In the SCI patient population, the AE profile for the 300U dose group was similar to the 200U dose group.
Interpretation of Results
The results of this 4-year, long-term multicenter study demonstrate that the improvements in UI, volume/void, and QOL following onabotulinumtoxinA 200U treatment are clinically meaningful and are sustained over a period of up to 4 years in patients with SCI. Discontinuation rates due to AEs or lack of efficacy were low. These results further support the use of onabotulinumtoxinA in patients with SCI and NDO and UI who are not adequately managed by at least 1 anticholinergic medication.
Concluding Message
Repeat onabotulinumtoxinA treatment provided consistent improvement in UI and QOL in SCI patients with UI due to NDO who had not been adequately managed by at least 1 anticholinergic. OnabotulinumtoxinA 200U was well tolerated, with no new safety signals identified over 4 years’ follow-up.
Disclosures
Funding: Allergan, Inc. and Allergan, Ltd. Clinical Trial: Yes Registration Number: NCT00876447 RCT: No Subjects: HUMAN Ethics Committee: Institutional review boards (IRBs) and/or ethics committees at each individual study center Helsinki: Yes Informed Consent: Yes
1Carolinas Medical Center, Charlotte, NC, USA; 2St. Hedwig-Krankenhaus, Berlin, Germany; 3Vanderbilt University Medical Center, Nashville, TN, USA; 4University of Manitoba, Winnipeg, MB, Canada; 5Cleveland Clinic Main Campus, Cleveland, OH, USA; 6Allergan, Inc., Bridgewater, NJ, USA; 7Allergan, Ltd., Marlow, UK; 8Allergan, Inc., Irvine, CA, USA; 1Aix-Marseille Université, Marseille, France


