Dissected female porcine bladders were mounted in a modified Hysteroscopy Diagnostic Trainer. Using routine endoscopic equipment for this procedure with video monitoring, 6 urologists (experts group) and 6 urology trainees (novices group) completed UBA injections on a total of 12 bladders using ENI simulator. Face and content validities were assessed by using structured quantitative survey which rating the realism. Construct validity was assessed by comparing the performance, time of the procedure, and the occlusive (anatomical and functional) evaluations between the experts and novices. Trainees also completed a post-procedure feedback survey. Effective injections were evaluated by measuring the retrograde urethral opening pressure, visual cystoscopic coaptation, and post-procedure gross anatomic examination.

Figure 1: Dissected Female Porcine Bladders were Mounted in a Modified Hysteroscopy Diagnostic Trainer
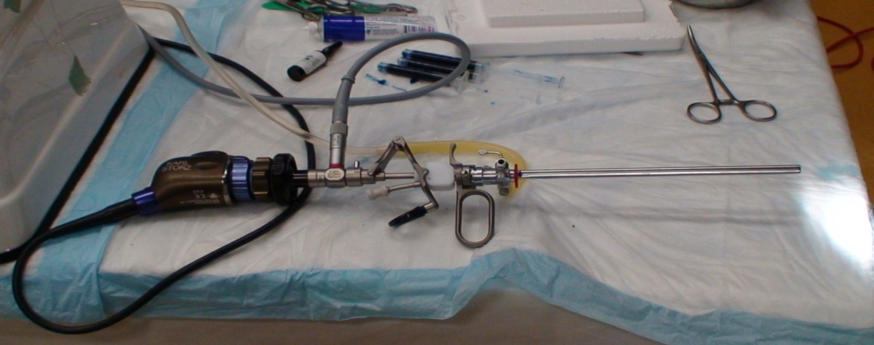
Figure 2: Cystoscopy and Injection Set Up

Figure 3: The syringe filled with the mixed methylene blue (or other dye, such as indigo carmine) and surgical lubricant. The syringe’s Luer lock fits on to the needle. All needles will be primed before the residents initiate injection.
All 12 participants felt the simulator was a good training tool and should be used as essential part of urology training (face validity). ENI simulator showed good face and content validity with average score varies between the experts and the novices were 3.9/5 and 3.8/5 respectively. Content validity evaluation showed that most aspects of the simulator were adequately realistic (mean Likert scores 3.9-3.8/5). However, the bladder does not bleed, and sometimes thin. Experts significantly outperformed novices (P<001) across all measure of performance, therefore, establishing construct validity.
Our study provides evidence to support the continuing use of the UCI ENI simulator in urology training as it clearly showed face, content, and construct validities. Although few aspects of the simulator were not very realistic, it was considered a good training model. This study provides a basis for the future formal validation for this simulator with an expansion of the sample size and could be used to develop a performance-based training curriculum.
Written by: Bilal Farhan, MD; and Gamal Ghoniem, MD, FACS, University of California, Irvine, USA
Read the Abstract


