Due to the lack of evidence-based information that emphasizes differences between surgical and alternative techniques, the aim of our systematic review and meta-analysis was to evaluate the efficacy and safety of bulking agents compared with surgical methods for the treatment of female SUI.4
We conducted an electronic search from 2000 to 2021 in PubMed, MEDLINE, and the Cochrane Library with keywords and MeSH terms: “bulking agents,” “stress urinary incontinence,” and “surgery”. According to PICO criteria, only female patients with SUI were included. Therefore, the primary analysis aimed to assess objective and/or subjective success in achieving better continence and quality of life of women with SUI. The secondary analysis was aimed at safety assessment based on the classification by Dindo et al.5
Our electronic database search yielded 950 publications. Only six were included in the final analysis, compliant with 710 patients, 288 in the urethral bulking agent group, and 317 in the surgery group. According to the Cochrane Handbook, two reviewers assessed the risk of bias of each of the studies included using RoB 2 for randomized control trials and ROBINS-I for nonrandomized trials. The overall risk of bias for nonrandomized trials was critical. Based on the RoB 2 tool, randomized trials had equal low and high-risk possibilities, and the summary plot indicated some concerns regarding the overall risk of bias.
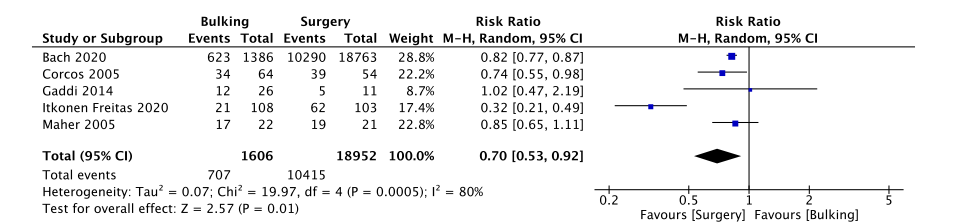
The primary analysis was focused on subjective symptom improvement 12 months after the intervention. In this meta-analysis, 5 out of 6 studies were included: (RR = 0.70, 95% CI: 0.53 to 0.92, p = 0.01). Consequently, surgical treatment showed effectiveness over bulking agents in the subjective improvement of SUI symptoms.
Fig. 1 Primary outcome—comparison between subjective improvement in patients after bulking agent versus surgery
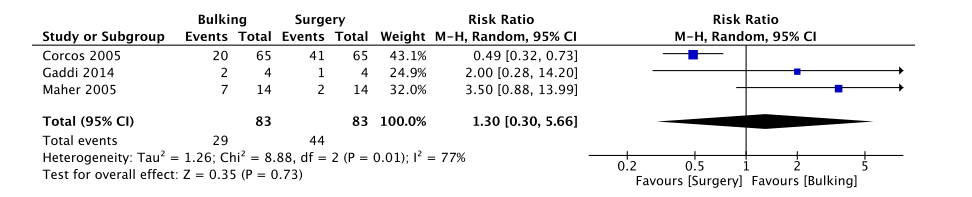
The secondary analysis was aimed at safety and complications during SUI treatment according to the classification by Dindo et al. Only grade 3 complications were included. In this meta-analysis, 3 out of 6 studies were involved: (RR = 1.30, 95% CI: 0.30 to 5.66, p = 0.73). As a result, there was no statistically significant difference between bulking agents and surgery complications during treatment.
Fig.2 Secondary outcome—comparison between complications in patients after bulking agent versus surgery (grade 3 according to the classification by Dindo et al.)
Implications for future research may include a comparison of bulking agents and mid-urethral slings and an evaluation of the quality of life (measured using one standard questionnaire), objective symptoms before and after treatment (with a standard follow-up of 12 months), and intra−/postoperative complications (with the same follow-up period). A well-performed study design with standard outcome measures and a complete follow-up period will help scientists and healthcare professionals be more confident in choosing different options for the SUI treatment.
In conclusion, our systematic review and meta-analysis show that bulking agents are less effective than surgical procedures based on subjective improvement after treatment. Additionally, there is no statistically significant difference in complications after the intervention between these two methods. Hence, we believe that the first and final surgery is considered to be the best.
Written by: Laura Pivazyan,1 George Kasyan,2 Bagrat Grigoryan1 & Dmitry Pushkar2
- First Moscow State Medical University by I.M. Sechenov (Sechenov University), Moscow, Russian Federation
- Urology Department, Moscow State University of Medicine and Dentistry, Moscow, Russian Federation
References:
- Dyer O. Johnson and Johnson faces lawsuit over vaginal mesh devices. BMJ. 2016;353:i3045. https://doi.org/10.1136/bmj.i3045.
- Keltie K, Elneil S, Monga A, et al. Complications following vaginal mesh procedures for stress urinary incontinence: an 8-year study of 92,246 women. Sci Rep. 2017;7:12015. https://doi.org/10.1038/s41598-017-11821-w.
- US Food and Drug Administration, FDA. US Food and Drug Administration Executive Summary: reclassification of urogynecologic surgical mesh instrumentation. http://www.fda. gov/downloads/AdvisoryCommittees/ .
- Pivazyan, L., Kasyan, G., Grigoryan, B., & Pushkar, D. (2021). Effectiveness and safety of bulking agents versus surgical methods in women with stress urinary incontinence: a systematic review and meta-analysis. International urogynecology journal, 10.1007/s00192-021-04937-1. Advance online publication. https://doi.org/10.1007/s00192-021-04937-1
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.


