In the classical description of the VEIL procedure, the initial dissection plane is superficial, just below the Scarpa’s fascia. This blind dissection offers little control in the absence of a distinct plane and often results in a variable thickness skin flap leading to flap-related complications. In the described modified approach, the initial dissection plane is deep, just over the fascia lata, which is a distinct tough layer and allows better control during initial dissection [Image 1].4 The cavity thus formed allows direct visualization of the dissection limits, important surgical landmarks, and direct access to the saphenous vein close to the saphenofemoral junction early in the course of surgery [Image 2]. Dissection in the superficial plane is done after the deep dissection and is entirely under direct vision, with better dissection control.
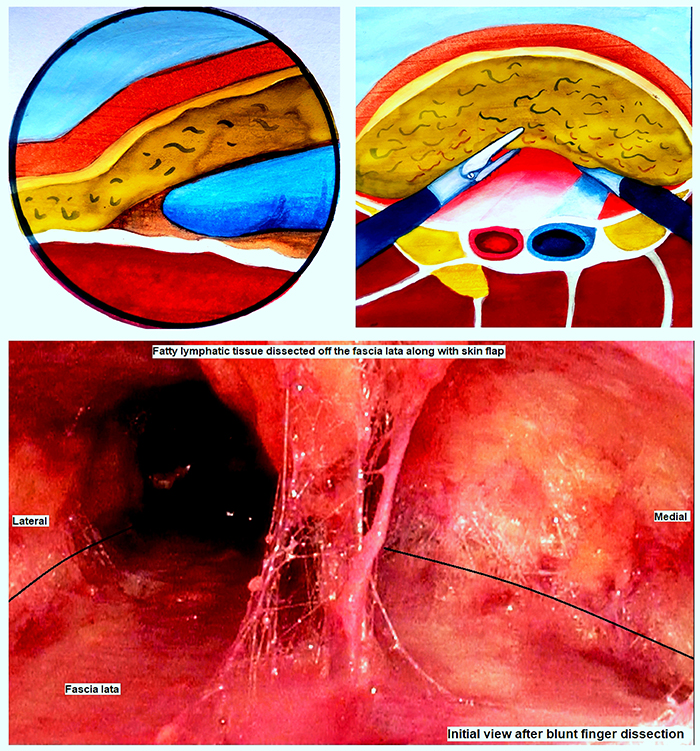
Image 1: The “initial deep dissection plane” developed over the fascia lata using blunt finger dissection (Top left). The deep-dissection cavity allows early visualization of the dissection limits and critical vascular structures (Top right). The initial endoscopic view of the deep-first approach shows the fatty lymphatic tissue dissected from the fascia lata (Bottom). The dissection plane is visualized laterally and medially (marked with a black line).
After a decade of the first description, acceptance of the VEIL procedure is impeded by poor ergonomics of operating in a small cavity. While the robotic-assisted approach eliminates the concerns of poor ergonomics, there is still space for pure laparoscopic procedures. Even with the robotic-assisted approach, the initial dissection is still done blindly. The described modified deep-first approach may improve the learning curve and ergonomics of the VEIL procedure.
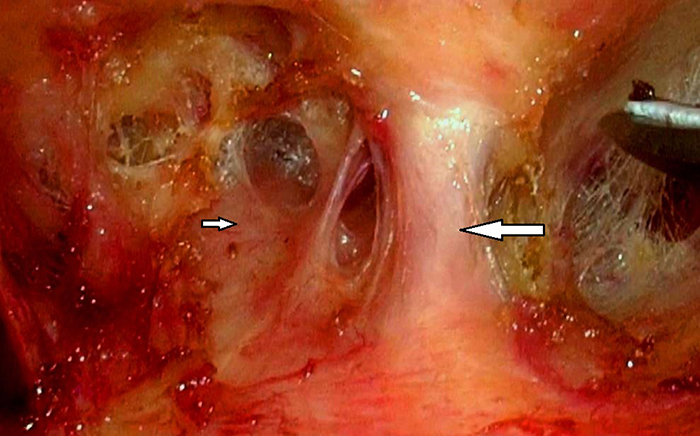
Image 2: Saphenous vein (large arrow) visualized close to the saphenofemoral junction, with the femoral artery (small arrow) just lateral to it.
Written by: Abhishek Pandey,1 Manoj K. Das,2 Swarnendu Mandal,2 Prasant Nayak,3 Santosh Kumaraswamy1
- Urology Resident, Department of Urology, All India Institute of Medical Sciences, Bhubaneswar, India
- Assistant Professor, Department of Urology, All India Institute of Medical Sciences, Bhubaneswar, India
- Additional Professor and Head of department, Department of Urology, All India Institute of Medical Sciences, Bhubaneswar, India
References:
- Hakenberg OW, Compérat E, Minhas S, Necchi A, Protzel C, Watkin N. EAU Guidelines on Penile Cancer. EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam 2022. ISBN 978-94-92671-16-5. EAU Guidelines Office, Arnhem, The Netherlands. Available from: https://uroweb.org/guidelines/penile-cancer/chapter/disease-management
- Stuiver MM, Djajadiningrat RS, Graafland NM, Vincent AD, Lucas C, Horenblas S. Early wound complications after inguinal lymphadenectomy in penile cancer: a historical cohort study and risk-factor analysis. Eur Urol. 2013 Sep;64(3):486–92.
- Tobias-Machado M, Tavares A, Ornellas AA, Molina WR, Juliano RV, Wroclawski ER. Video Endoscopic Inguinal Lymphadenectomy: A New Minimally Invasive Procedure for Radical Management of Inguinal Nodes in Patients With Penile Squamous Cell Carcinoma. Journal of Urology. 2007 Mar;177(3):953–8.
- Das MK, Pandey A, Mandal S, Nayak P, Kumaraswamy S. Modified Video Endoscopic Inguinal Lymphadenectomy: a deep-first approach. Urology. 2022 Jun 17.
Read the Abstract


