To evaluate the effects from different penumbra settings, some standard comparisons are made, including 95% volume does, critical structure doses, hot and cold spots at target, and dose profile at target. At 95% volume dose point, no significant difference can be observed for every penumbra setting, see Figure 1. Siemen Primus and Primart gave slightly larger dose at critical structures. An interesting point was observed in Fig. 1 at the hot spot examinations, which shows larger hot spots from Varian 21Ex, while Varian 21Ex has the smallest penumbra among the three linac models. To evaluate the possibility of the plan with larger hot spots, we calculated the percentage of the hot spots at each case in the overall dose delivery. The largest hot spot from Varian’s to Siemens linacs is 1.5% of the target volume. The penumbra comparisons provide us an important perspective on explaining the hot spots in the target (PTV) for the Varian linac and the hot spots in the rectum for the Siemens linac models. In order to trace where the hot spots come from, target (CTV) DVHs are also drawn, and the hot spots are smaller compared to the PTV DVHs. This indicates the hot spots take place in the margin between the CTV and the PTV, which is the radiation beam penumbra region. From the dose profile at the target observation, the calculations with Varian 21 Ex setting showed the more heterogeneous dose distributions at the irradiation area than other two machines, see Figure 2.
In order to verify the penumbra-induced hot spot effect, we delivered the same plan with different artificial penumbra settings, including 3.5cm, 2.9cm, 2.2cm 1.5cm, and 0cm penumbra value at 100 cm SSD. The DVH of these five cases are shown in Figure 3. It shows that as we expected to see that smaller penumbra will have better coverage at target and lower dose at critical structures; however, 0cm and 1.5cm penumbra setting show a larger hot and cold spots than 2.2cm setting, and hot spots than 2.9, and 3.5cm settings. This suggests that a penumbra of 2.2cm at 100cm SSD is the optimal setting for this plan. This can also explain why the Varian 21 Ex can have larger target dose heterogeneity with the smallest penumbra.
Therefore, smaller MLC leaves may improve dose conformity but introduce more target dose heterogeneity. The hot spots can be partially explained by the overlapping of MLC segments while larger beam penumbra can smear out the overlapping effect. An optimal beam penumbra can lead to the best target dose uniformity.
Figure 1. DVH comparisons between Varian 21Ex, Siemens Primus and Primart for prostate PTV and rectum.
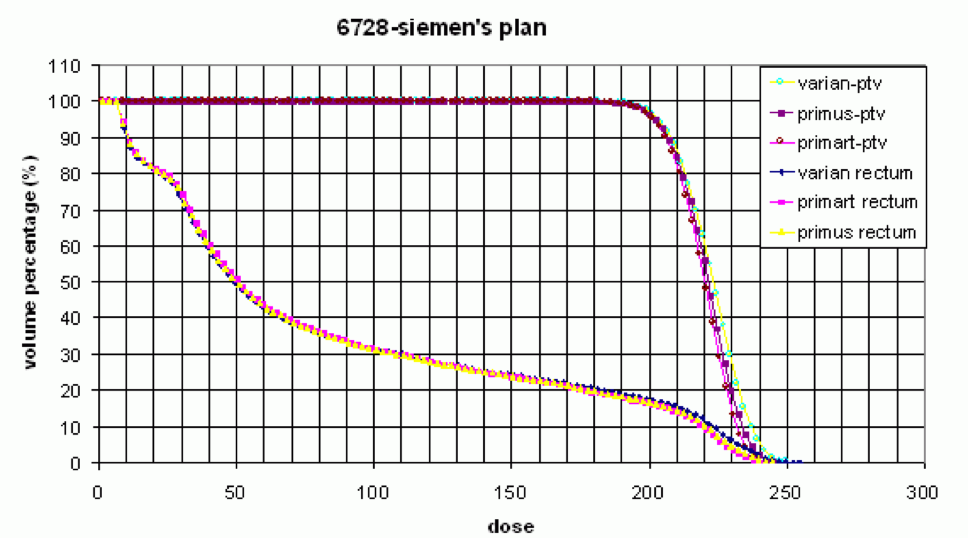
Figure 2. Dose distributions at isocenter plane (a) larger penumbra; (b) smaller penumbra.

Figure 3. DVH comparison of penumbra setting with 3.5cm, 2.9cm, 2.2cm 1.5cm, and 0cm at 100cm SSD.

Written by:
Teh Lin, PhD, DABR, Assistant Professor / Medical Physicist, Fox Chase Cancer Center, Radiation Oncology Department Philadelphia, PA
Read the Abstract


