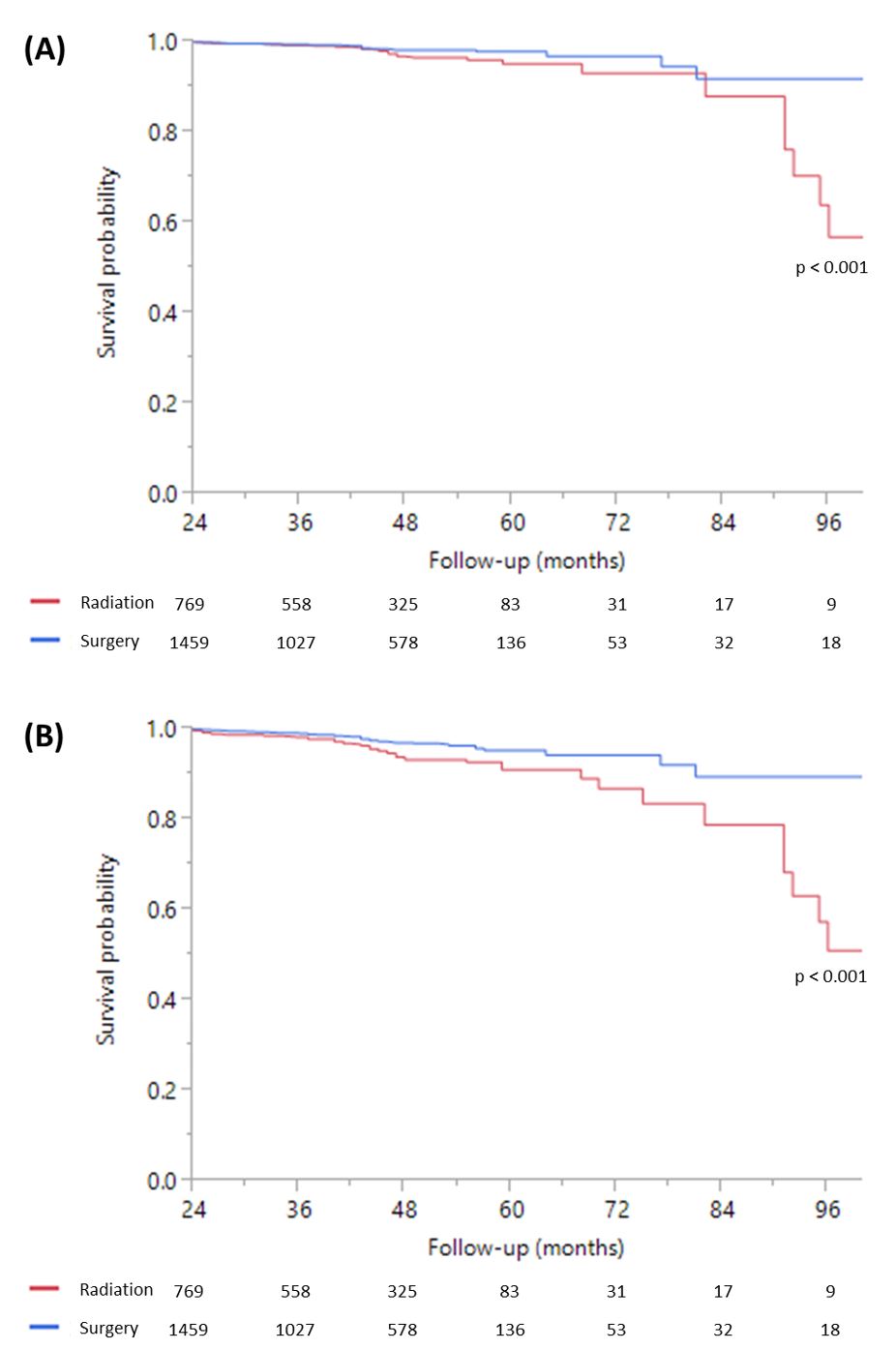
Figure 1. Kaplan-Meier survival curve for (A) prostate cancer-specific mortality and (B) overall mortality in patients with localized high-grade prostate cancer treated with initial surgery vs. radiation
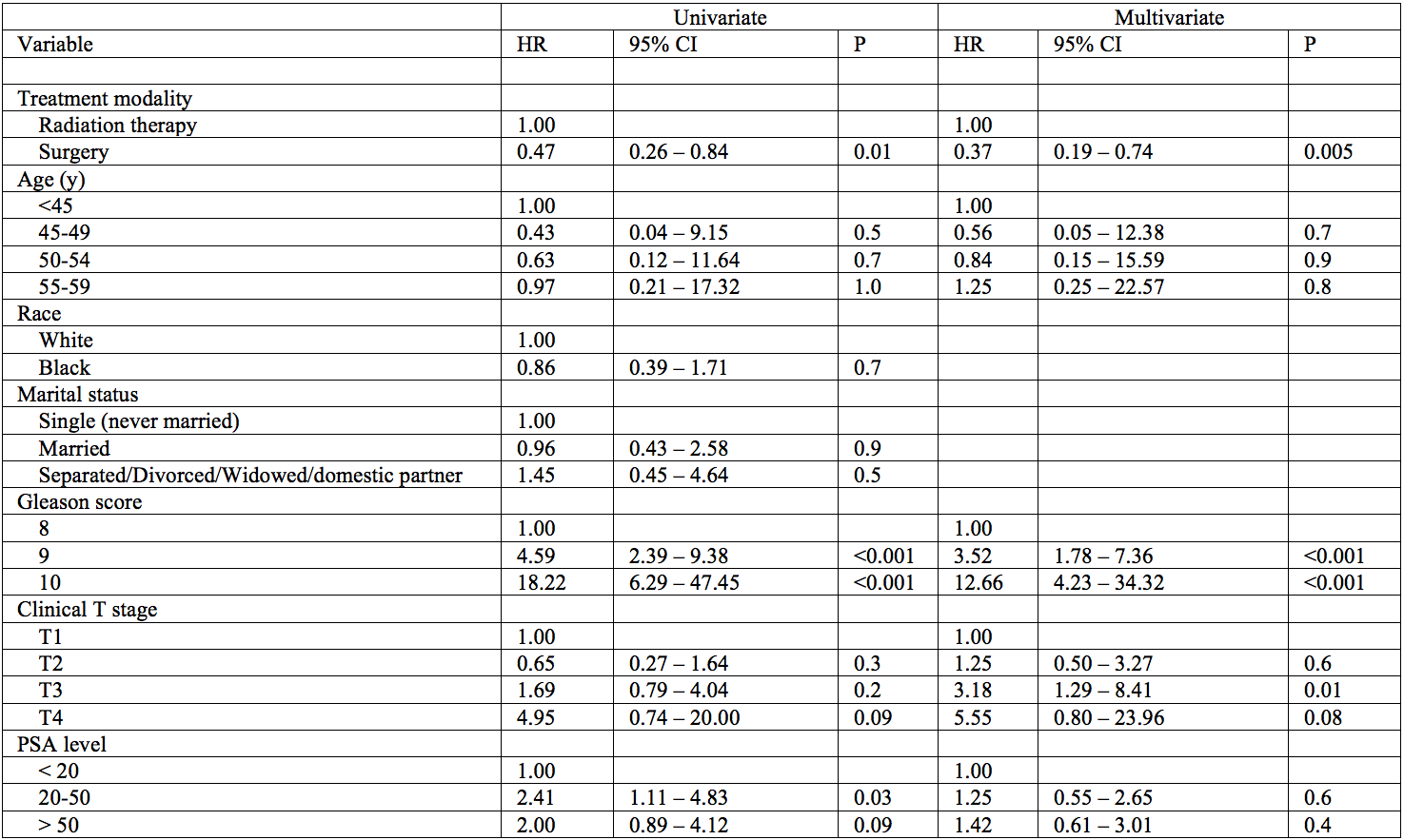
Table 1. Univariate and Multivariate Cox proportional hazards models of prostate cancer-specific mortality for primary treatment with surgery vs. radiation therapy
These improved mortality outcomes by the surgery arm were confirmed using inverse-probability treatment weighting analysis (HR 0.28, 95% CI 0.17 – 0.46, p < 0.001 and HR 0.57, 95% CI 0.43 – 0.76, p < 0.001). We also performed subgroup analyses to compare outcomes of men treated with initial surgery, external beam radiation therapy (EBRT), and combination external beam radiation therapy with brachytherapy (EBRT+BT). We found no significant difference in prostate cancer-specific mortality (HR 0.74, 95% CI 0.26 – 1.86, p = 0.5) between the EBRT and EBRT+BT groups, but EBRT+BT was associated with reduced overall mortality versus EBRT alone (HR 0.40, 95% CI 0.15 – 0.89, p = 0.02). Comparison of EBRT+BT and RP groups did not show any significant difference in prostate cancer-specific and overall mortality (HR 0.41, 95% CI 0.13 – 1.65, p = 0.2 and HR 0.96, 95% CI 0.31 – 4.10, p = 0.9).
Our study represents a contemporary source of evidence comparing survival outcomes in RP vs RT for a younger cohort. Due to its retrospective nature and reliance on a cancer registry, further prospective studies are needed to confirm these results.
A few noteworthy points are worth mentioning. First, our analysis showed that EBRT+BT was superior to EBRT alone for overall mortality but not cancer-specific mortality in our analysis. Recent data has shown that brachytherapy provides benefit in terms of disease recurrence. The ASCENDE-RT trial, which compared dose-escalated EBRT vs EBRT with low-dose rate brachytherapy boost in high-risk prostate cancer, showed that men treated with EBRT alone were twice as likely to experience a biochemical recurrence than those treated with EBRT+BT.2 In addition, multiple non-comparative series have reported favorable outcomes with brachytherapy boost.3 However, there are currently no randomized trials comparing survival outcomes of brachytherapy boost with contemporary dose-escalated EBRT.3 Second, we found no significant differences in survival outcomes between surgery and EBRT+BT. This is in contrast to a recent multi-institutional observational study by Kishan et al. with Gleason 9-10 cancer, which demonstrated that men treated with EBRT+BT had lower prostate cancer-specific and all-cause mortality than both surgery and EBRT groups at 7.5 years of follow-up.4
In our study, we acknowledge that splitting the RT arm into an EBRT and EBRT+BT group may not be sufficiently powered for a comparison between EBRT+BT and RP, as our EBRT+BT group made up 8.3% of our total sample size. Despite this limitation, without evidence from a randomized trial, it is still uncertain whether EBRT+BT will show improved outcomes compared to surgery. Until prospective randomized trials are completed to confirm the long-term outcomes of these treatment approaches, further observational studies should be pursued to elucidate the existing data.
Written By: Hubert Huang and Mohummad Minhaj Siddiqui M.D., Division of Urology, Department of Surgery, University of Maryland Medical Center, Baltimore, Maryland
Read the Abstract
References:
1. Huang H, Muscatelli S, Naslund M et al: Evaluation of Cancer-Specific Mortality with Surgery Versus Radiation as Primary Therapy for Localized High-Grade Prostate Cancer in Men Younger than 60 Years Old. J Urol 2018.
2. Morris WJ, Tyldesley S, Rodda S et al: Androgen Suppression Combined with Elective Nodal and Dose Escalated Radiation Therapy (the ASCENDE-RT Trial): An Analysis of Survival Endpoints for a Randomized Trial Comparing a Low-Dose-Rate Brachytherapy Boost to a Dose-Escalated External Beam Boost for High- and Intermediate-risk Prostate Cancer. Int J Radiat Oncol Biol Phys 2017; 98: 275.
3. Mendez LC, Morton GC: High dose-rate brachytherapy in the treatment of prostate cancer. Transl Androl Urol 2018; 7: 357.
4. Kishan AU, Cook RR, Ciezki JP et al: Radical Prostatectomy, External Beam Radiotherapy, or External Beam Radiotherapy With Brachytherapy Boost and Disease Progression and Mortality in Patients With Gleason Score 9-10 Prostate Cancer. JAMA 2018; 319: 896.


