Many urologists use nomograms in the office to help their patients with elevated PSA decide if a biopsy is necessary, but the question of how to figure out if your patient fits into that small percentage of patients with significant prostate cancer persists. Addressing one of the biggest concerns with prostate MRI, missed lesions, Dr. Chapin argues that those were unlikely to be clinically significant and may have still been identified in the future without deleterious effect on outcomes. The PROMIS trial1 compared the accuracy of MRI with systematic TRUS biopsy, finding that a negative MRI missed 3% of significant cancers, however, TRUS biopsy alone missed 21%.
Furthermore, when MRI screening determined whether or not a biopsy should be performed, 27% of biopsies would have been avoided. The findings of this study challenge the role of prostate biopsy as the gold standard for prostate cancer diagnosis. In a recent randomized trial, (PRECISION 2) MRI screening reduced detection of insignificant prostate cancers while also improving detection of cancers with Gleason 3+4 or above. Finally, though MRI may at first appear to increase costs associated with prostate cancer diagnosis, cost-modeling has projected that the reduction in unnecessary diagnosis and treatment more than compensates for this increase.


Biopsy First
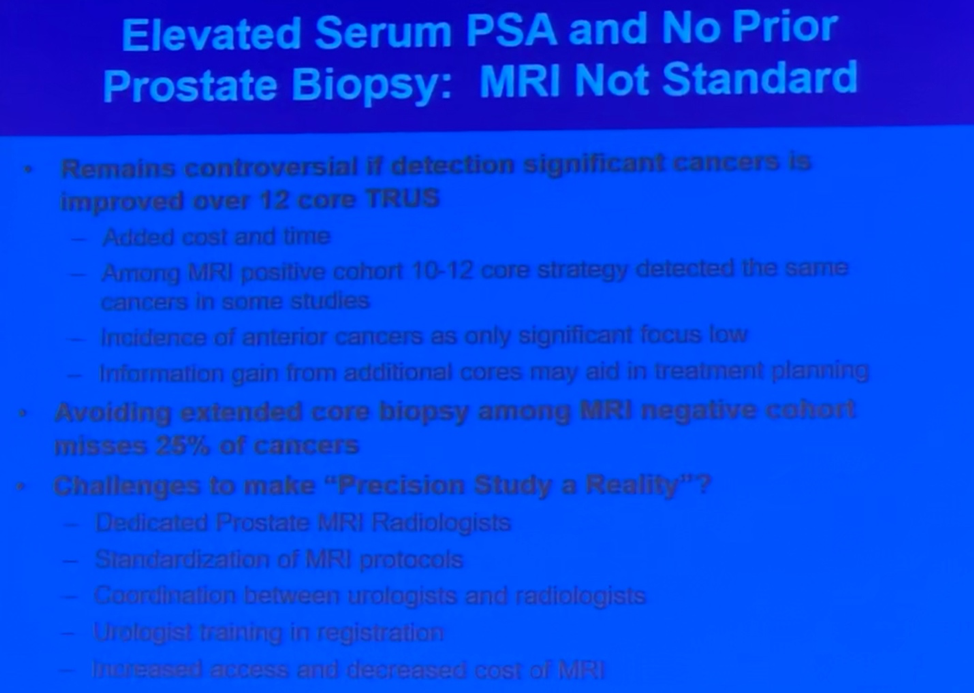
Dr. Pettaway agrees with the overall goal of limiting prostate cancer detection to only the “clinically significant” tumors while avoiding over-diagnosis and treatment. What should be noted upfront is that none of the leading guidelines currently support the addition of prostate MRI for determining which patients should be considered for prostate biopsy. MRI may be useful for finding tumors in patients with persistently elevated PSA who have a lesion in an anatomically difficult location (i.e. anterior) but the increased detection is only seen in the context of a prior negative biopsy. Returning to the PRECISION trial, Dr. Pettaway acknowledges the remarkable results in favor of MRI, however, calls into question the generalizability for widespread use. The radiologists were prostate MRI experts, yet concordance was only 70%. Additionally, MRI prompted biopsy patients did not have systematic biopsy and may have missed further significant cancer in a patient that was otherwise deemed negative. Furthermore, multiple RCTs have shown that MRI for use in fusion biopsy is no better than a systematic approach3, 4.
Presented by: Brian F. Chapin, MD, and Curtis A. Pettaway, MD, Department of Urology, University of Texas MD Anderson Cancer Center, Houston, TX, USA
Written by Justin T. Matulay, MD, Urologic Oncology Fellow and Ashish M. Kamat, MD (@UroDocAsh), Professor, Department of Urology, Division of Surgery, The University of Texas MD Anderson Cancer Center, Houston, TX at the 13th Update on the Management of Genitourinary Malignancies, The University of Texas (MDACC - MD Anderson Cancer Center) November 9-10, 2018, Dan L. Duncan Building, Houston, TX
References
1. Ahmed, H.U., A. El-Shater Bosaily, L.C. Brown, et al., Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet, 2017. 389(10071): p. 815-822.
2. Kasivisvanathan, V., A.S. Rannikko, M. Borghi, et al., MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med, 2018. 378(19): p. 1767-1777.
3. Radtke, J.P., C. Schwab, M.B. Wolf, et al., Multiparametric Magnetic Resonance Imaging (MRI) and MRI-Transrectal Ultrasound Fusion Biopsy for Index Tumor Detection: Correlation with Radical Prostatectomy Specimen. Eur Urol, 2016. 70(5): p. 846-853.
4. Baco, E., E. Rud, L.M. Eri, et al., A Randomized Controlled Trial To Assess and Compare the Outcomes of Two-core Prostate Biopsy Guided by Fused Magnetic Resonance and Transrectal Ultrasound Images and Traditional 12-core Systematic Biopsy. Eur Urol, 2016. 69(1): p. 149-56.


