Costs of prostate cancer care are estimated to approach $12 billion a year, and the actual numbers are likely higher. Costs of brachytherapy (Perlroth 2011) are likely around $14,000, comparing relatively favorably to surgery. Reasons to choose brachytherapy include the fact that surrounding organs are relatively insulated compared with external beam radiotherapy, high doses can be reliably administered, the procedure can be performed as a single treatment (for the low dose rate), and the procedure is performed as an outpatient. Candidates for brachytherapy alone include low volume intermediate-risk patients, and brachytherapy plus EBRT can be offered to intermediate risk (high volume) and high-risk patients. Dr. Anscher noted that over time, the utilization of brachytherapy has decreased, in part because provider training for the procedure has lessened.
Dr. Anscher promotes three principles for improving brachytherapy: first, incorporation of better imaging, including efforts to use MRI-based programs to define the prostate more accurately (Frank et al, Brachytherapy 2017). Second, strategies to protect normal tissue can be included, such as the use of products such as the SpaceOAR hydrogel, which can be injected into the space between the prostate and the rectum to minimize radiation exposure to the rectum. Finally, appropriate patient selection, including avoiding treatment of very low-risk prostate cancer cases, and staging appropriately, is important.
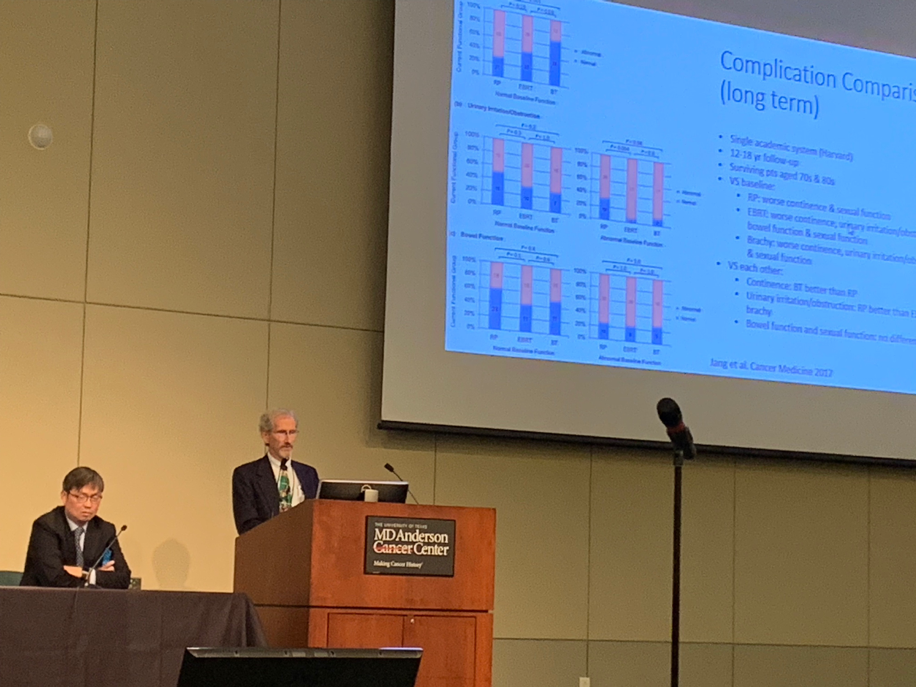
Dr. Seungaek Choi spoke about the use of hypofractionated intensity-modulated radiation therapy (IMRT) as another approach to treating localized prostate cancer. Dr. Choi noted that the hypothesis of the efficacy of hypofractionated therapy relies on the fact that prostate cancer cells are known to have a low alpha/Beta ratio, thus permitting dose-escalation through hypofractionation. Why use hypofractionated treatment? According to Dr. Choi, patients often select this modality because it is less invasive. Some studies have also shown that there may be cost advantages. Hypofractionated treatment has been incorporated into the ASTRO guidelines and is an effective and safe option for the treatment of prostate cancer; it can be considered standard of care, for both low and intermediate prostate cancer. As with brachytherapy, patient selection is key, with patients with smaller prostates and lower AUA symptom scores favored for therapy.
Presented by: Mitchell S. Anscher, MD, Professor, Radiation Oncology, and Seungtaek Choi, Associate Professor, Radiation Oncology, University of Texas MD Anderson Cancer Center, Houston, Texas
Written by: Dr. Vikram M. Narayan (@VikramNarayan), Urologic Oncology Fellow and Ashish M. Kamat, MD (@UroDocAsh), Professor, Department of Urology, Division of Surgery, The University of Texas MD Anderson Cancer Center, Houston, TX at the 13th Update on the Management of Genitourinary Malignancies, The University of Texas (MDACC - MD Anderson Cancer Center) November 9-10, 2018, Dan L. Duncan Building, Houston, TX


