There are circumstances in which these modalities have a distinct advantage over the conventional methods of investigations such as computed tomography or bone scintigraphy. In a biochemical recurrence setting after primary treatment, PSMA PET has been found to have a high detection rate of metastatic lesions even at a low PSA of <0.5ng/ml. In the PCa screening population, mpMRI has been shown to have high sensitivity and negative predictive value for clinically significant PCa. In addition, mpMRI and PSMA PET may both be used in place of prostate biopsy in patients with contraindications for biopsy such as irreversible coagulopathy, rectal pathology, previous rectal operations including anterior-perineal resection or immuno-compromisation. PSMA PET can be also used in patients with renal impairment as the ligands are not nephrotoxic. Nevertheless, these promising novel technologies have significant limitations and they should be appreciated.
Figure 1 depicts a case that outlines the potential benefits and disadvantages of these imaging modalities. In a patient with biochemical recurrence post radical prostatectomy, bladder neck recurrence was visualized by mpMRI (image A and B), whilst PSMA PET (image C and D) did not identify the recurrence. The implications were that the use of salvage treatment could be different according to the imaging tests used.
Whilst emerging clinical trials are incorporating the novel imaging modalities into the study protocols, there is limited availability of prospective mature data. Until the long-term implications of the use of the novel technologies and the health economic data are made available, patients should be made aware of the potential benefits and harms related to these technologies. Until then, a multi-disciplinary team consisting of urological surgeons, radiation oncologists, medical oncologists, radiologist, nuclear medicine physician, nurses, and allied health professionals have a strong role in discussing and reviewing the outcomes of any novel investigations prior to deviating from a standard of care pathway based on the findings of the tests.
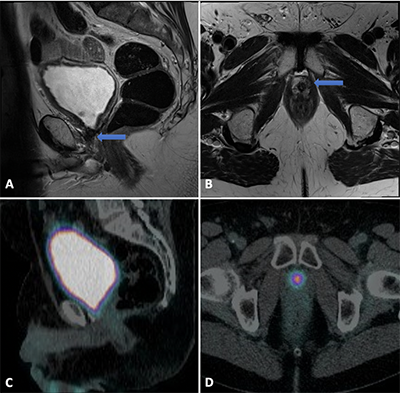
Figure 1. Bladder Neck Recurrence After Surgery Defined By MRI. Pelvic image of 62 year old with BCR of PSA at 0.5ng/ml after radical prostatectomy. MRI of pelvis identified T2 hypointense area at the bladder neck antero-laterally (blue arrow): A) Sagittal; and B) Axial planes. A biopsy confirmed the diagnosis of local recurrence using MR/US guided biopsy. PSMA PET did not identify the tumour either due to the halo-effect of the accumulated contrast in the bladder or due to the inability of the tumour to produce PSMA expression. PSMA PET: C) Sagittal; and D) Axial planes.
Written by: Margaret Mansbridge, BMSc, MBBS, Eric Chung, FRACS (Urol), and Handoo Rhee, PhD Candidate, APCRC-Q, Urology Research Fellow, Princess Alexandra Hospital, Department of Urology, Princess Alexandra Hospital, Woolloongabba, Australia, Department of Urology, Princess Alexandra Hospital, Woolloongabba, Australia
Read the Abstract


