Like RP, radiation can be successful when Gleason grade groups 2-4 are present, but often fails in men with Gleason group 5 disease. These men can have disease that is resistant to standard doses of radiation or cancers that have spread outside of the gland. In an evaluation of 99 patients, Narang et al. found similar inferior outcomes as RP when very high-risk prostate cancer was present.3 At 10 years, 56.6% had a biochemical failure and 13.2% had died of prostate cancer when conventional radiation doses were used. When a brachytherapy boost is added to external beam irradiation therapy (combination therapy) the total dose of radiation can be as much as 30% higher than intensity-modulated radiation therapy (IMRT) alone. The brachytherapy boost also provides a higher dose of radiation outside of the prostate. In a 2017 report the American Brachytherapy Society task group reviewed 39 publications in men with high-risk prostate cancer treated by RP, (external beam radiation therapy) EBRT and combination therapy.4 Ten-year biochemical relapse-free survival ranged from 27-68% for RP, 37-55% for EBRT and 54-93% for combination therapy.
Stone recently reported on 2742 men treated at Mount Sinai Hospital (New York, NY, USA, n = 2277) and at The Brachytherapy Center at Hygeia Hospital (Athens, Greece, n = 465) that were enrolled in a prospective database for patients with prostate cancer treated by permanent seed implant.5 Of 2742, 320 (11.7%) men were identified that had either Gleason group 4 (n=186) or Gleason group 5 (n=134) prostate cancer. Treatment consisted of neoadjuvant hormonal therapy (median nine months), I-125 (planning dose 110 Gy) or Pd-103 (planning dose 100 Gy) followed one month later by 45 Gy of external beam irradiation. Postimplant dosimetry was performed using computed tomography-based dosimetric analysis with radiation doses converted to the biological equivalent radiation dose (BED) with an α/β of 2 using the D90 metric. The BED was dichotomized to < 200 Gy vs. > 200 Gy based on prior reporting.6
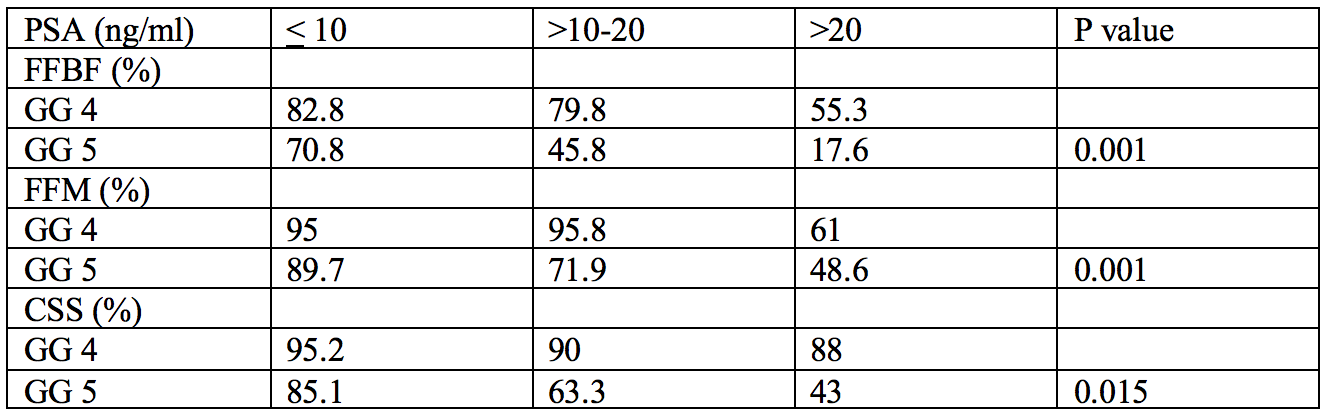
Ten-year freedom from biochemical failure for Gleason group 4 and 5 was 76.5 vs 61.3% (p=0.015); freedom from metastases was 93.5 vs. 83.8% (p=0.006) and cause-specific survival was 94 vs. 79.3% (p=0.001) (figures 1-3).

Figure 1. Five- and 10-year freedom from biochemical failure (Phoenix definition) for Gleason group 4 vs. 5. Numbers represent patients remaining
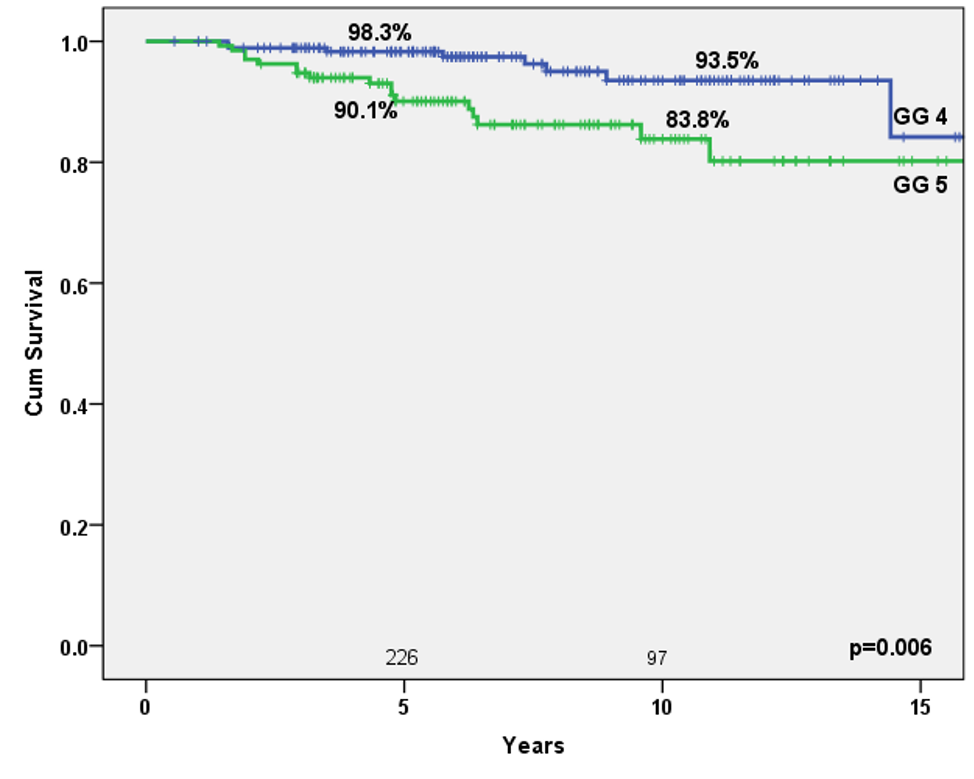
Figure 2. Five- and 10-year freedom from metastatic disease for Gleason group 4 and 5 disease
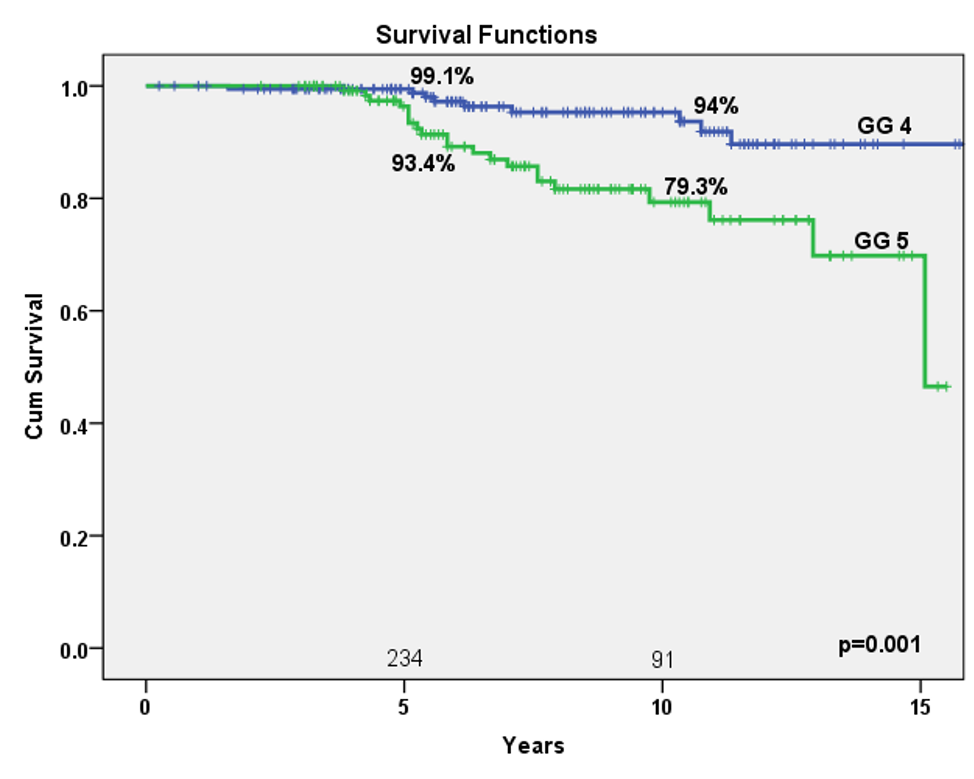
Figure 3. Five- and 10-year cause-specific survival for Gleason group 4 and 5 disease.
When BED was dichotomized to < 200 Gy vs > 200 Gy biochemical failure occurred in 37/110 (33.6%) vs 37/197 (18.8%, OR 2.2, 95% confidence interval [CI] 1.3-3.7, p=0.004) and prostate cancer mortality was 17/110 (15.5%) vs. 14/197 (7.1%%, OR 2.4, 95% 1.1-5.1, p=0.020). Increased PSA was associated with worse biochemical failure, increased metastases prostate cancer mortality for both Gleason group 4 and 5 (table 1).
Table 1. Ten-year freedom from biochemical failure (FFBF), freedom from metastases (FFM), cause-specific failure (CSS) by PSA value.
Data from several studies suggest that most men with Gleason group 5 prostate cancer will require multimodality therapy. Muralidhar compared brachytherapy boost with EBRT to RP plus adjuvant radiotherapy (RT) from the NCDB (National Cancer Database) and the SEER databases.7 In 6643 patients, the five-year overall survival and prostate cancer mortality between RP and brachytherapy boost was no different for the two treatments (86.7% vs 87.0%, p=0.220 and 6.0% vs 5.7%, p=0.234).
A BED > 200 Gy should be considered the standard dose when treating men with Gleason group 4 and 5 disease with radiotherapy. A radiation dose of this amount conferred an improvement in biochemical control of 2x and half the number of prostate cancer deaths over lower doses. When compared to an IMRT dose of 79-81 Gy, a BED of 200 Gy has a biological equivalence of 108 Gy of EBRT which may help explain why standard doses of EBRT are associated with higher failure rates. It is important for clinicians to recognize that all combination therapy is not equal and that a post implant D90 of at least 110 Gy for I-125 or 100 Gy for Pd-103 combined with 45 Gy (25 fractions of 1.8 Gy) EBRT (assuming an ꭤ/β of 2) is necessary to achieve this BED. In addition, when Gleason grade group 4 and 5 prostate cancer is found early (PSA < 10 ng/ml), men who are given radiation with a BED > 200 Gy have 10-year cause-specific survival > 85%. These data also underscore the benefit of early detection in men with high-grade disease.
Written by: Nelson N. Stone, MD, Professor of Urology and Radiation Oncology, The Icahn School of Medicine at Mount Sinai, New York, New York
References:
- Pierorazio, Phillip M., Thomas J. Guzzo, Misop Han, Trinity J. Bivalacqua, Jonathan I. Epstein, Edward M. Schaeffer, Mark Schoenberg, Patrick C. Walsh, and Alan W. Partin. "Long-term survival after radical prostatectomy for men with high Gleason sum in pathologic specimen." Urology 76, no. 3 (2010): 715-721.
- Djaladat, Hooman, Erfan Amini, Weichen Xu, Jie Cai, Siamak Daneshmand, and Gary Lieskovsky. "Oncological outcomes after radical prostatectomy for high‐risk prostate cancer based on new Gleason grouping system: a validation study from University of Southern California with 3,755 cases." The Prostate 77, no. 7 (2017): 743-748.
- Narang, Amol K., Carol Gergis, Scott P. Robertson, Pei He, Ashwin N. Ram, Todd R. McNutt, Emily Griffith et al. "Very high-risk localized prostate cancer: outcomes following definitive radiation." International Journal of Radiation Oncology* Biology* Physics 94, no. 2 (2016): 254-262.
- Spratt, Daniel E., Payal D. Soni, Patrick W. McLaughlin, Gregory S. Merrick, Richard G. Stock, John C. Blasko, and Michael J. Zelefsky. "American Brachytherapy Society Task Group Report: Combination of brachytherapy and external beam radiation for high-risk prostate cancer." Brachytherapy 16, no. 1 (2017): 1-12.
- Stone, Nelson N., Vassilios Skouteris, and Richard G. Stock. "Long-term biochemical control and cause-specific survival in men with Gleason grade Group 4 and 5 prostate cancer treated with brachytherapy and external beam irradiation." Brachytherapy (2020).
- Stock, Richard G., Nelson N. Stone, Jamie A. Cesaretti, and Barry S. Rosenstein. "Biologically effective dose values for prostate brachytherapy: effects on PSA failure and posttreatment biopsy results." International Journal of Radiation Oncology* Biology* Physics 64, no. 2 (2006): 527-533.
- Muralidhar, Vinayak, Brandon A. Mahal, Santino Butler, Nayan Lamba, David D. Yang, Jonathan Leeman, Anthony V. D'Amico et al. "Combined external beam radiation therapy and brachytherapy versus radical prostatectomy with adjuvant radiation therapy for Gleason 9-10 prostate cancer." The Journal of urology 202, no. 5 (2019): 973-978.


