In staging, PET/MRI showed a high pooled sensitivity for the detection of primary cancer in the prostate gland, mainly at patient-based analysis. In one study, extracapsular spread of prostate cancer was detected better with 68Ga-PSMA PET/MRI than with mpMRI. In another study, PET and PET/MRI produced a considerably lower proportion of equivocal results (i.e. PIRADS 3) than mpMRI. The pooled sensitivity for lymph-node metastasis was about 65% (Table 1).
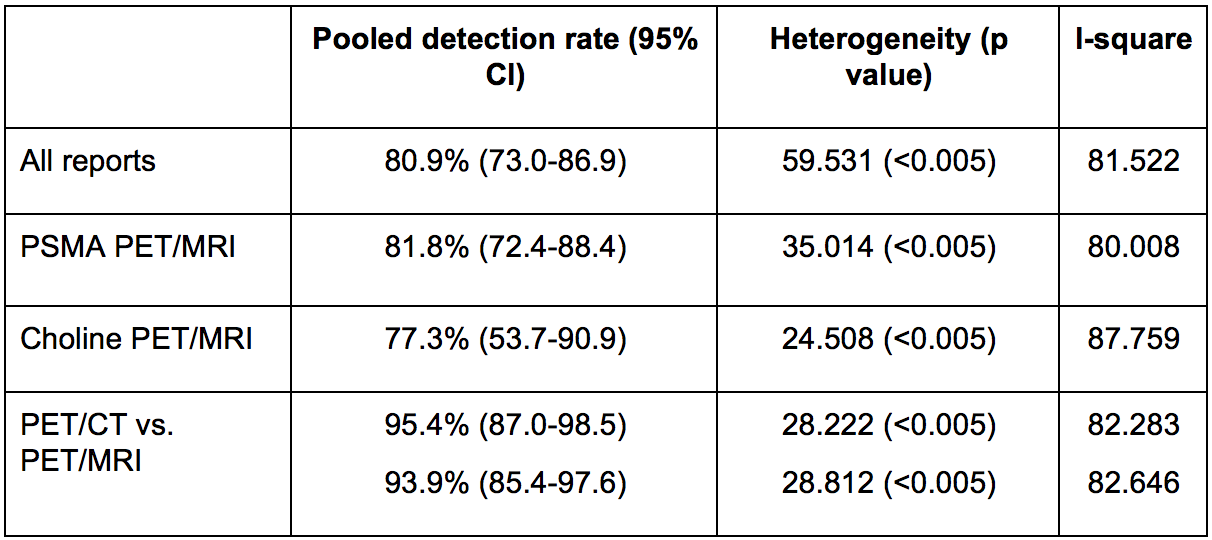
In the biochemical recurrence setting, PET/MRI reported a detection rate ranging between 54.5% and 97%. The detection rate was higher in accordance with PSA levels. The pooled detection rate was 81%. It was higher for studies using radiolabelled PSMA than choline (82 vs. 77 %, respectively). In the studies that compared PET/CT with PET/MRI in the same population, the pooled detection rates were similar. However, in some studies, PET/MRI was superior to PET/CT in detecting primary prostate malignant lesions, particularly in cases of local recurrence with low prostate-specific antigen (PSA) levels (Table 2). Furthermore, PET/MRI achieved a slightly higher detection rate in recurrent lymph-node disease. Finally, the detection rate of bone metastasis was comparable between PET/CT and PET/MRI in the case of PSA <2 ng/ml, but PET/CT performed better with PSA levels > 2 ng/ml. This result suggests the implementation of specific bone sequences in PET/MRI.
Table 1. Pooled sensitivity and specificity for staging
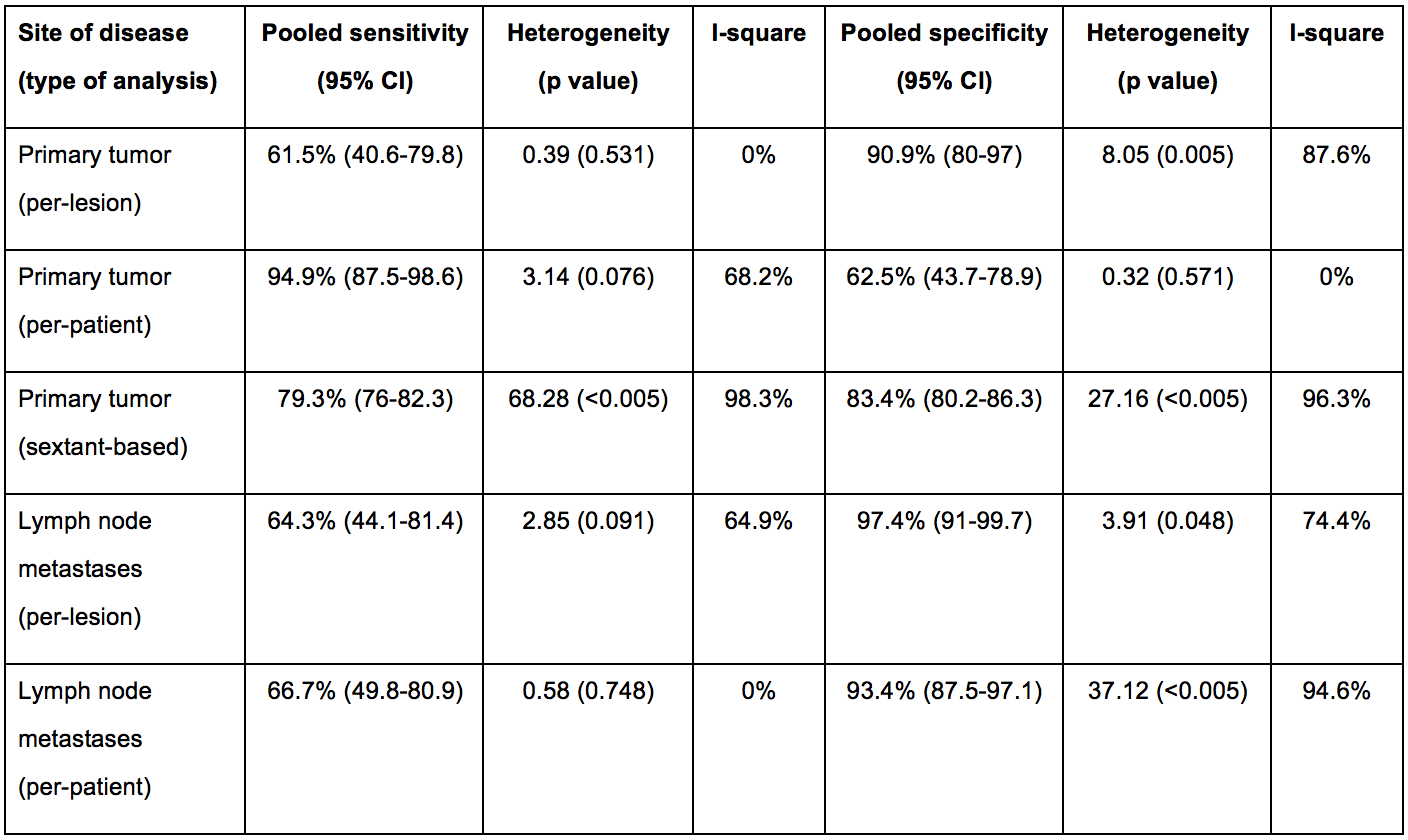
Table 2. Pooled detection rate in restaging
Finally, therapeutic strategies were modified in at least 30% of patients in staging, while it prompted changes in up to 75% of cases in restaging, for example by identifying oligometastatic disease and thus guiding to the appropriate radiotherapeutic planning.
Written by: Laura Evangelista, Fabio Zattoni, Gianluca Cassarino, Paolo Artioli, Diego Cecchin, Fabrizio Dal Moro, Pietro Zucchetta
Nuclear Medicine Unit, Department of Medicine, Padova University Hospital, Via Giustiniani 2, Padova, Italy., Urology Unit, Department of Medicine, Udine University Hospital, Udine, Italy., Nuclear Medicine Unit, Department of Medicine, Padova University Hospital, Via Giustiniani 2, Padova, Italy.
Read the Abstract


