There is an increasing debate as to whether technical variants of examination using fewer MRI sequences can achieve similar diagnostic accuracy while mitigating the above-mentioned limitations. Several studies showed promising results when investigating the accuracy of “abbreviated MRI protocols” in detecting clinically significant PCa,4 but intra-individual direct comparison of multiple technical variants in the same study cohort has been rarely performed.5 Thus, it is unclear which “abbreviated” MRI variant better approximates mpMRI, and, in turn, to which extent a single mpMRI examination can be shortened. Indeed, one might assume that saving even a few minutes on a per-examination basis over a large number of patients can significantly decrease indirect costs, and increase the accessibility of prostate MRI. For instance, by saving 4 minutes every 10 patients, one might save 40 minutes in all, which roughly corresponds to the acquisition time of one average examination. Thus, saving 4 minutes can translate into performing one new examination per 10-patients, i.e. 100 new examinations/1000 patients. This is of paramount importance in an era requiring even more prostate MRI examinations in biopsy-naïve patients according to current recommendations.6
Our Institutional Review Board approved study aimed to compare the cancer detection rate (CDR) for clinically significant PCa of mpMRI and multiple abbreviated MRI protocols in a cohort of patients who underwent radical prostatectomy (RP). Of note, having used final pathology after RP as the standard of reference might have represented a more robust standard of reference than biopsy, as the latter carries the risk of inflating the CDR by not accounting for undetected false-negatives.
We retrospectively included 108 men who underwent preoperative staging of biopsy-proven PCa at our Institution in the period 01/2016 – 05/2019. Patients underwent mpMRI on a 3.0T magnet, using a PI-RADS-compliant mpMRI protocol that has been further optimized with local physicists. Two radiologists (R1 and R2), blinded to clinical information and final pathology, independently reviewed each mpMRI examination according to the reading order shown in Figure 1, and using the PI-RADS version 2 (PI-RADSv2) for reporting each of the sequences separately. A study coordinator provided the final PI-RADS categorization of observations by combining the per-sequence PI-RADS categories according to the illustrated combinations, which correspond to four different MRI protocols: mpMRI, biparametric MRI (bpMRI), short MRI (sMRI), and contrast-enhanced short MRI (cesMRI). Based on the matching with final pathology, we calculated the per-lesion CDR (number of correctly identified clinically significant cancers divided by total number of clinically significant cancers), false discovery rate (FDR, number of false-positive observations divided by total number of positive observations) using PI-RADSv2 category 3 or higher as the cut-off. Clinically significant PCa was defined according to Epstein criteria.
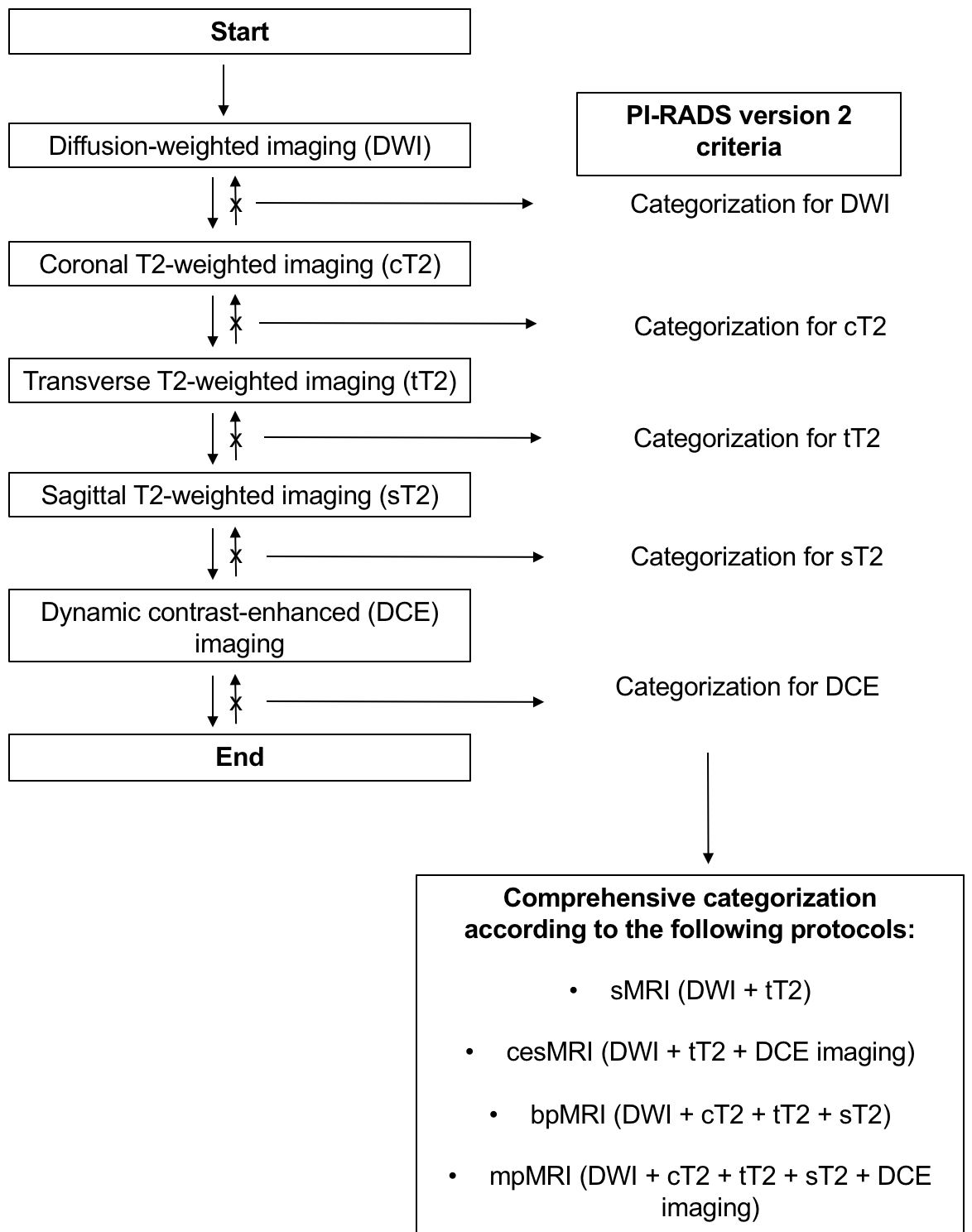
Figure 1. Flowchart illustrating the imaging analysis strategy for achieving final PI-RADS categorization of findings according to different combinations of mp-MRI derived sequences.
The pathological analysis found 142 clinically significant cancers in 108 men. We observed comparable CDR for the MRI protocols, with no significant inter-reader difference on a per-protocol basis (p = 0.199 for both sMRI and cesMRI, and p = 0.143 for both bpMRI and mpMRI). FDR was similar across the four protocols, i.e. 14.4%-14.5% for R1, and 11.1% for R2.
Of note, cesMRI decreased category 3 assignments compared to sMRI, since most of them were upgraded to PI-RADSv2 4 category (11/24 and 9/12 for R1 and R2, respectively), with most upgraded and non-upgraded observations consisting of true positives cases, i.e. 6/11 and 10/13 cases for R1, and 8/9 and 3/3 cases for R2, respectively. Thus, although sMRI was the protocol with the fewest sequences equaling mpMRI, cesMRI decreased the prevalence of clinically significant PCa within PI-RADSv2 3 observations (66.7% versus 76.9% for R1, and 91.7% versus 100% for R2), as well as the FDR (23.1% versus 33.3% for R1, and 0% versus 8.3% for R2, respectively). An example case is shown in Fig. 2.

Figure 2. Prostate magnetic resonance imaging (MRI) of a 76-year-old man with an International Society of Urological Pathology grade group 2 cancer in the left posterior peripheral zone at the level of the mid-gland (prostate-specific antigen [PSA] level of 7.8 ng/mL). A focal observation with ambiguous restriction of diffusion (slightly hyperintensity on ultra-high b-value [a] and hypointensity on the ADC map [b]), corresponding to a hypointense focus on transverse T2-weighted imaging (c), thus leading to a PI-RADS 3 assignment, is evident. On DCE (d) the observation showed intense focal contrast-enhancement, upgrading the observation to a PI-RADS 4 assignment. Overall, while there was no difference between short MRI (sequences on a, b, and c) and contrast-enhanced MRI (sequences on a-d) in terms of cancer detection, the use of contrast medium helped to increase the suspicion of disease and more properly categorizing the finding as PI-RADS 4.
Despite the main limitation of having derived the abbreviated protocols from the same mpMRI examination, our study showed that shorter variants (sMRI and cesMRI) performed comparably to mpMRI in detecting clinically significant PCa. Although sMRI was the minimum array of sequences approximating mpMRI, adding DCE imaging led to the fewest PI-RADSv2 3 assignments, most of which were true positives. Thus, cesMRI can be advocated as the best-abbreviated protocol to minimize false-positive PI-RADSv2 category 3 observations, thus reducing the risk of unnecessary biopsies. In conclusion, even in the context of abbreviated MRI, the use of contrast medium is, apparently, still useful.
Written by: Gianluca Giannarini, MD,1 Rossano Girometti, MD2,3
- Urology Unit, Academic Medical Centre “Santa Maria della Misericordia”, Udine, Italy
- Institute of Radiology, Academic Medical Centre “Santa Maria della Misericordia”, Udine, Italy
- Department of Medicine, University of Udine, Academic Medical Centre “Santa Maria della Misericordia”, Udine, Italy
- Girometti, Rossano, Lorenzo Cereser, Filippo Bonato, and Chiara Zuiani. "Evolution of prostate MRI: from multiparametric standard to less-is-better and different-is better strategies." European Radiology Experimental 3, no. 1 (2019): 5.
- De Visschere, Pieter JL, Alberto Briganti, Jurgen J. Fütterer, Pirus Ghadjar, Hendrik Isbarn, Christophe Massard, Piet Ost et al. "Role of multiparametric magnetic resonance imaging in early detection of prostate cancer." Insights into imaging 7, no. 2 (2016): 205-214.
- de Rooij, Maarten, Esther HJ Hamoen, J. Alfred Witjes, Jelle O. Barentsz, and Maroeska M. Rovers. "Accuracy of magnetic resonance imaging for local staging of prostate cancer: a diagnostic meta-analysis." European urology 70, no. 2 (2016): 233-245.
- Padhani, Anwar R., Ivo Schoots, and Geert Villeirs. "Contrast medium or no contrast medium for prostate cancer diagnosis. That is the question." Journal of Magnetic Resonance Imaging 53, no. 1 (2021): 13-22.
- van der Leest, Marloes, Bas Israel, Erik Bastiaan Cornel, Patrik Zamecnik, Ivo G. Schoots, Hans van der Lelij, Anwar R. Padhani et al. "High diagnostic performance of short magnetic resonance imaging protocols for prostate cancer detection in biopsy-naïve men: the next step in magnetic resonance imaging accessibility." European urology 76, no. 5 (2019): 574-581.


