
Figure 2. A: Pi-RADS 3a (≤0.5 ml); B: Pi-RADS 3b (>0.5 ml)
Recently, we published a series of prostate biopsies2 with prior magnetic resonance imaging (MRI) and evaluated the association between the results of the MRI and the prostate-specific antigen (PSA) density (PSAd) value and observed that, with a cut-off point of 0.15, the negative predictive value of clinically significant prostate cancer (csCaP) detection in negatives or equivocal (Pi-RADS 1, 2, and 3) MRI was increased by 100%.
In this study, we evaluated all transperineal prostate biopsies performed between 2015 and 2020 in the Hospital Alemán of Buenos Aires, Argentina. The aim of it was to evaluate the association of the volume of the Pi-RADS 3 lesions and the PSAd in the diagnosis of csCaP. We evaluated the sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) considering 3b as positive for the detection of csCaP and when adding the PSAd value. We excluded those patients with no previous MRI and those who presented a negative or positive result in the MRI (PI-RADS 1-2-4 and 5).
Ninety-nine patients were included. We subdivided the patients according to the PI-RADS 3 subclassification and the PSAd value and defined the csCaP as Gleason score ≥3+4 or ≥ISUP2. Patients’ mean age was 64.1±7.19 years and median PSA was 7.28±2.6 ng/ml. The median prostate size estimated by MRI was 55.3±13.1 ml.
We found that patients with Pi-RADS 3a lesions did not present csCaP and 17.8% (10 patients) with Pi-RADS 3b lesions did. Furthermore, results in the Pi-RADS 3a lesions subgroup are shown regardless of PSAd value. In the 3b with PSAd > 0.15 group, 62.5% of cases presented csCaP. In 3a with PSAd > 0.15 group and also in the PSAd ≤ 0.15 group, no csCaP was found; therefore, 43 biopsies could have been avoided. In group 3b with PSAd≤0.15, all biopsies were isCaP and 40 biopsies could have been avoided. In total, only the 3b with PSAd > 0.15 group presented csCaP and 83.8% (83/99) biopsies could have been avoided. Considering 3b as positive for csCaP detection, sensitivity was 100%, specificity was 48.3%, negative predictive value (NPV) was 17.8%, and positive predictive value (PPV) was 100%. When adding PSAd to 3b group, sensitivity was 100%, specificity was 86.9%, NPV was 62.5%, and PPV was 100%.
Table 2. Results of the subdivision according the lesion size and PSAd
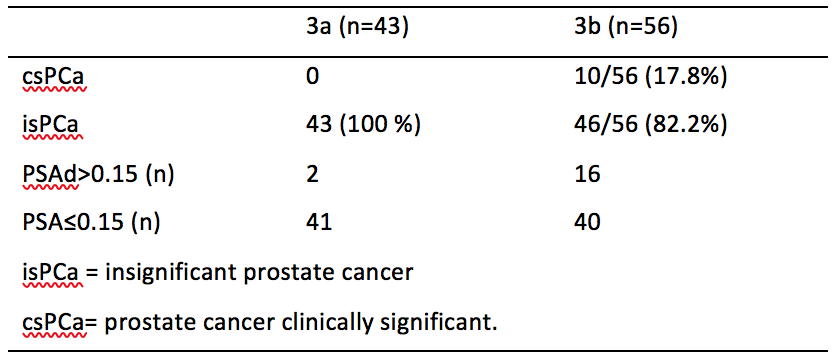
Table 3. csPca, according to PSAd and Pi-RADS 3 subclassification

In conclusion, the association of the volume of PIRADS 3 lesions and the PSAd increased specificity and PPV contributing to improving the early detection of csCaP.

Written by: Luis Rico, Leandro Blas, Gonzalo Vitagliano, Pablo Contreras, Hernando Rios Pita, Carlos Ameri
Hospital Aleman de Buenos Aires, Buenos Aires, Argentina.
References:
- Scialpi, Michele, Eugenio Martorana, Maria Cristina Aisa, Valeria Rondoni, Alfredo D’Andrea, and Giampaolo Bianchi. "Score 3 prostate lesions: a gray zone for PI-RADS v2." Turkish Journal of Urology 43, no. 3 (2017): 237.
- Rico, Luis, Pablo Contreras, Gonzalo Vitagliano, Hernando Rios Pita, Carlos Ameri, and Leandro Blas. "Value of prostate-specific antigen density in negative or equivocal lesions on multiparametric magnetic resonance imaging." Turkish Journal of Urology 46, no. 5 (2020): 367.


