In this study, we rigorously assessed the performance of an AI-based digital twin of a pathologist, vPatho, across 2603 histological images of prostate tissue stained with hematoxylin and eosin (H&E). Our investigation encompassed an in-depth analysis of factors contributing to tumor grade discordance between the vPatho system and six human pathologists, shedding light on both the potential utility and limitations of AI in this domain.
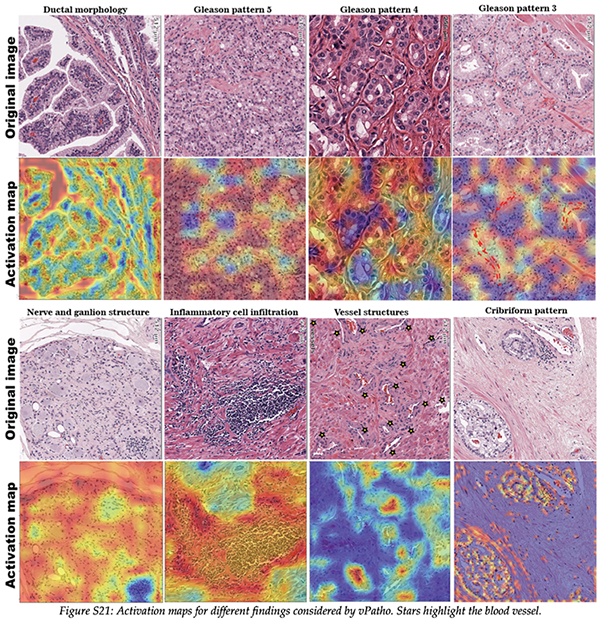
Our findings showed vPatho's accurate performance in detecting prostate cancer and estimating tumor volume, aligning with existing literature. Notably, vPatho exhibited moderate to substantial agreement with human pathologists in identifying complementary histological features such as ductal and cribriform morphologies, nerve and blood vessel involvement, and lymphocyte infiltration. However, concordance in tumor grading was reduced when applied to prostatectomy specimens compared to biopsy cores, prompting an exploration of potential solutions.
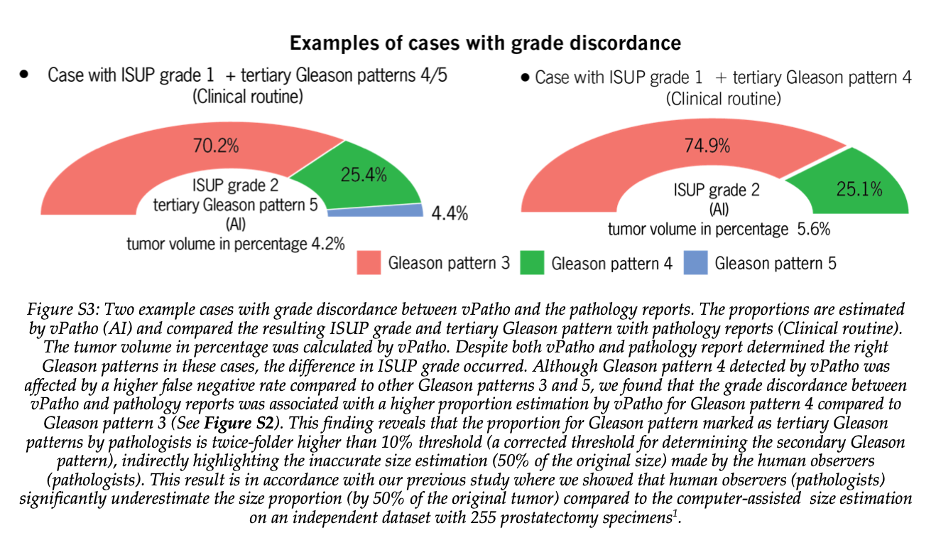
Addressing the observed grade discordance, we pinpointed several underlying challenges in applying the current grading system. These encompassed arbitrary decision thresholds for secondary Gleason patterns, cognitive biases affecting human pathologists, the impact of varying proportions of slides with prostate cancer, and the existence of a gray zone in ISUP grade groups. Proposals for mitigating these challenges included optimized thresholding algorithms and computer-aided proportion estimation techniques.
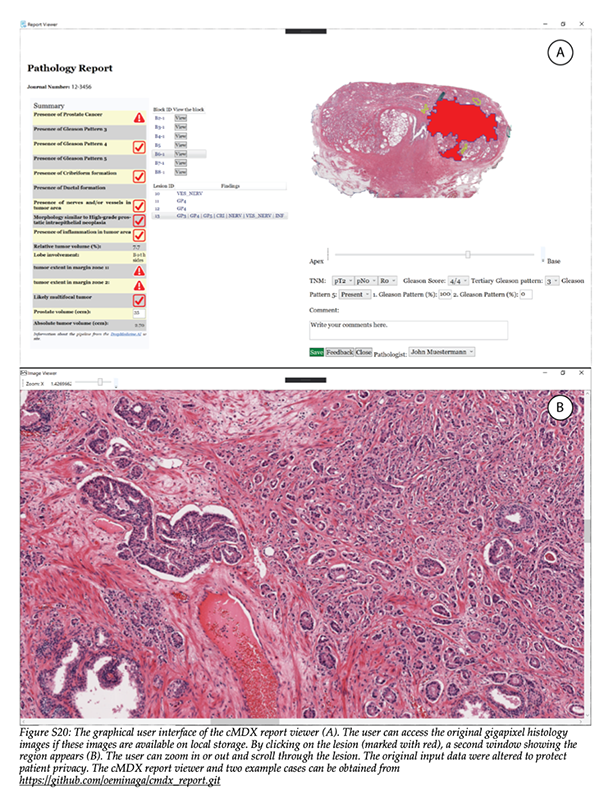
Moreover, our study delved into the importance of standardized test conditions and comprehensive evaluation practices, advocating for simulations that mirror real-world clinical scenarios. We emphasized the necessity of ongoing monitoring post-deployment to ensure AI integrity and regulatory compliance, underscoring the importance of replicating typical clinical conditions in testing frameworks.
Furthermore, we conducted a comparative analysis of our conclusions with geographically distinct studies, revealing varying levels of concordance among pathologists worldwide. This highlighted the complex interplay of social, cognitive, and geographic biases in pathology grading, urging for more standardized evaluation practices and AI solutions tailored to diverse clinical settings.
In conclusion, our study provides valuable insights into the potential of AI as a digital twin for pathologists in prostate cancer pathology. By elucidating existing limitations and proposing strategies for improvement, we pave the way for more effective AI integration in clinical practice, ultimately enhancing diagnostic accuracy and patient outcomes.
Finally, we highlight some figures showing interesting observations from our study that we hope the reader will enjoy.

Written by: Okyaz Eminaga, MD, PhD, AI Vobis, Palo Alto, CA
Read the Abstract


