Local treatments for the primary tumor have shown benefits in extending OS and postponing progression. However, disparities in clinical trial outcomes are notable; whereas the HORRAD trial1 failed to prove significant benefits of local radiotherapy (RT) in enhancing OS in newly diagnosed mHSPC, the STAMPEDE trial2 highlighted its substantial advantage in patients with low-volume disease. Additionally, evidence from population-based and cohort studies supports survival improvements with local interventions like cytoreductive radical prostatectomy (RP). Despite the potential of primary tumor treatments to mitigate local events, their definitive effectiveness in mHSPC patients is yet to be extensively studied.
On November 11, 2023, the PubMed, Scopus, and Web of Science databases were searched to identify studies investigating the effectiveness of local treatment of primary tumor for mHSPC to reduce local events. According to our inclusion criteria, we identified 2 RCTs, 2 prospective studies, and 2 retrospective studies with 3,565 patients eligible for meta-analyses.
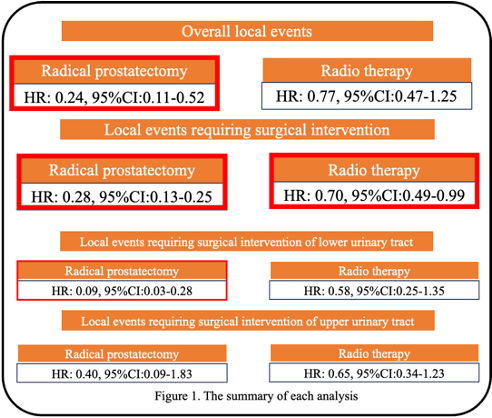
RP significantly reduced local event incidence (RR: 0.24, 95% CI: 0.11-0.52; Fig. 1), whereas RT did not show a significant difference in preventing overall local events (RR: 0.77, 95% CI: 0.47-1.25; Fig. 1). Both RP and RT significantly reduced local events requiring surgical intervention (RR: 0.08, 95% CI: 0.03-0.25, and RR: 0.70, 95% CI: 0.49-0.99; Fig. 1, respectively) RP significantly reduced the incidence of these events (RR: 0.09, 95% CI: 0.03-0.28; Fig. 1), while RT did not demonstrate a significant effect (RR: 0.58, 95% CI: 0.25-1.35; Fig. 1). Neither RP (RR: 0.40, 95% CI: 0.09-1.83; Fig. 1) nor RT (RR: 0.65, 95% CI: 0.34-1.23; Fig. 1) did show a significant effect on reduction of the incidence of upper urinary tract complications.
Written by: Ichiro Tsuboi, MD, Assistant Professor, Department of Urology, Shimane University Faculty of Medicine, Shimane, Japan; Department of Urology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan; Research Fellow, Department of Urology, Comprehensive Cancer Center, Medical University of Vienna, Vienna, Austria
References:
- Boevé LMS, Hulshof M, Vis AN, Zwinderman AH, Twisk JWR, Witjes WPJ, et al. Effect on Survival of Androgen Deprivation Therapy Alone Compared to Androgen Deprivation Therapy Combined with Concurrent Radiation Therapy to the Prostate in Patients with Primary Bone Metastatic Prostate Cancer in a Prospective Randomised Clinical Trial: Data from the HORRAD Trial.
- James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163-77. Epub 20151221. doi: 10.1016/s0140-6736(15)01037-5. PubMed PMID: 26719232; PubMed Central PMCID: PMCPMC4800035.


