Risk calculators that include MRI findings have been developed to predict individual risk of clinically significant prostate cancer (csPCa) and aid in biopsy decisions. These tools have become more important with their integration into the European Association of Urology's early detection guidelines. However, these models face challenges such as single-center designs, lack of sample size justification, and limited external validation.
The study aimed to validate and compare existing risk prediction models using a large, multicentric European cohort of patients who underwent MRI-targeted and systematic biopsies. Data from 4,841 patients from 15 European centers were analyzed. Pre-biopsy MRIs were performed following European guidelines and scored using PI-RADS v2 or 2.1 by expert radiologists. The biopsies were performed using the KOELIS system and analyzed by dedicated uropathologists.
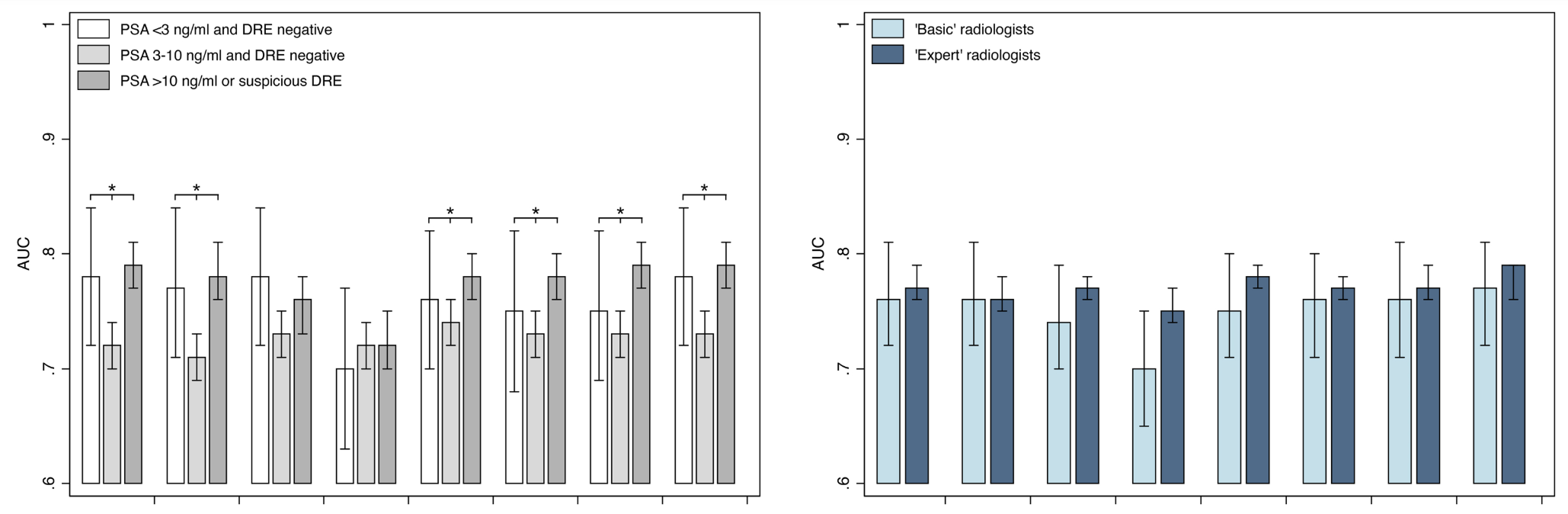
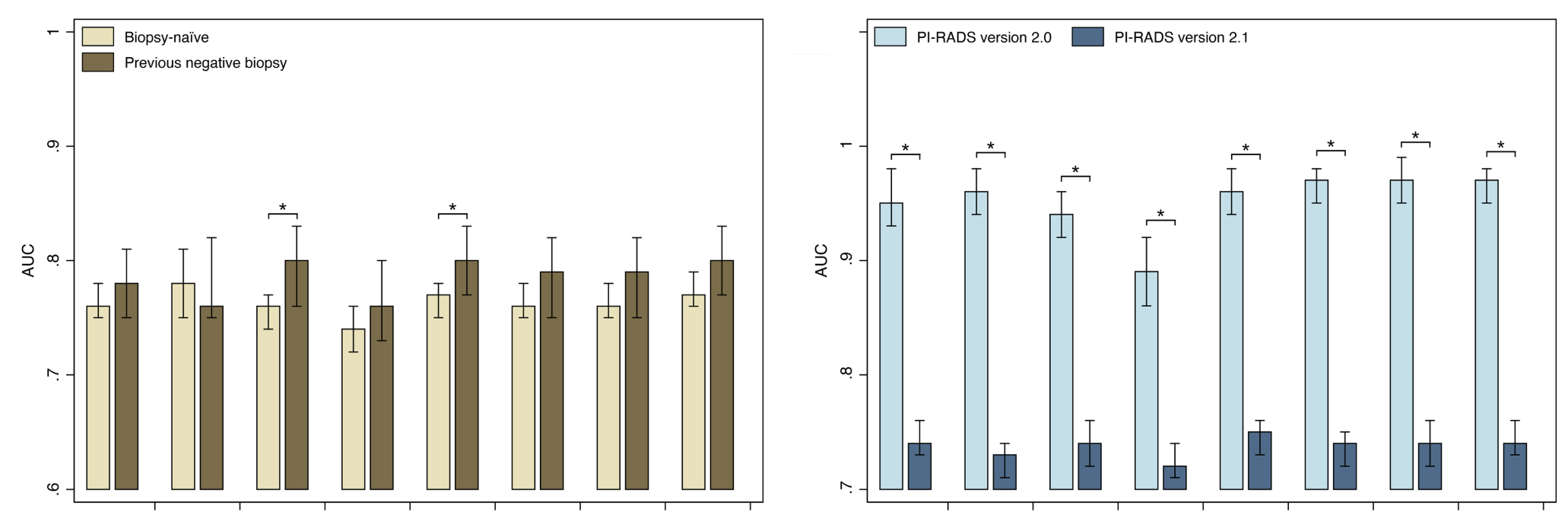
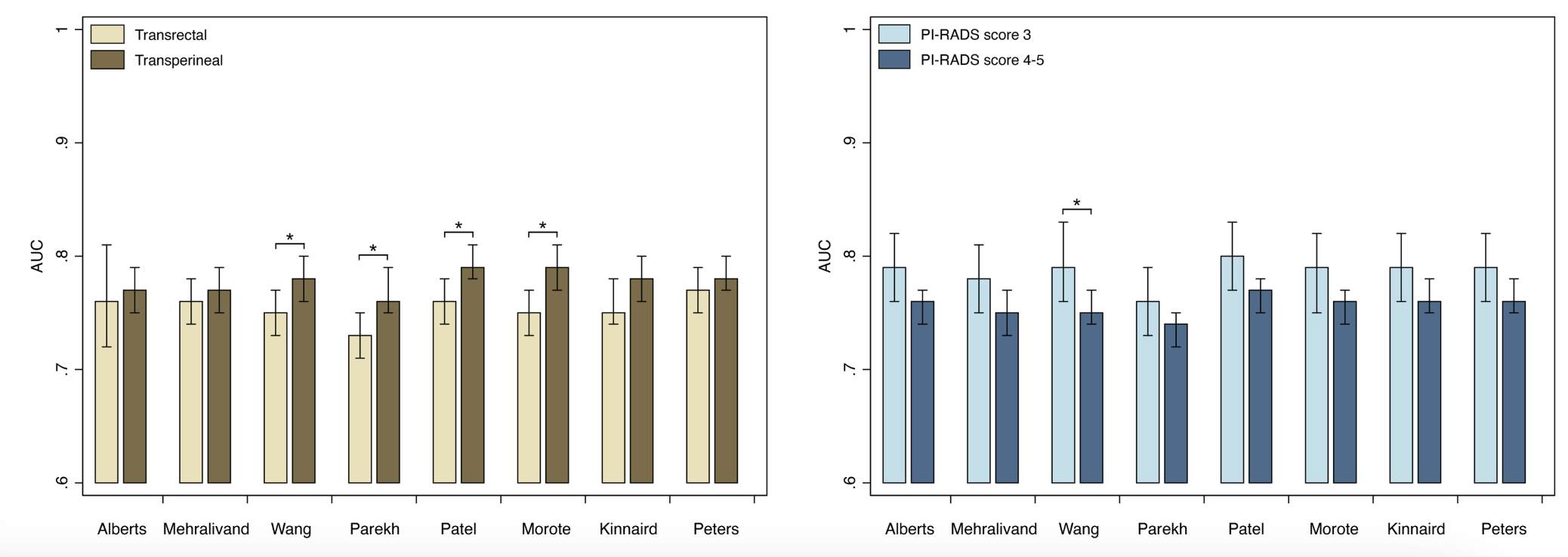
The study included eight predictive models, all incorporating MRI data. Statistical analysis assessed model performance in terms of discrimination, calibration, and net benefit. The models showed variable accuracy, with AUC values ranging from 0.75 to 0.78 (Figure 1). PI-RADS alone had an AUC of 0.53 for predicting csPCa. Models were less accurate for patients with PSA levels between 3-10 ng/ml and normal DRE. Models performed better when using PI-RADS v2 and transperineal biopsies.
The models showed increased net benefit for threshold probabilities above 10%, reducing unnecessary biopsies while minimizing missed csPCa cases. However, calibration and performance varied across different subgroups, and external validation highlighted the need for adjustments based on local csPCa prevalence.
In conclusion, the study validated eight models for predicting csPCa in patients with suspicious MRI lesions. The models showed adequate performance and clinical utility, particularly the Albert et al. model for threshold probabilities up to 20%. The findings emphasize the importance of updating models to reflect current guidelines and the need for careful consideration of local disease prevalence when applying these models in practice.
Written by: Romain Diamand, MD, PhD, FEBU, Department of Urology, Jules Bordet Institute, Hôpital Universitaire de Bruxelles, Université Libre de Bruxelles, Brussels, Belgium.
Read the Abstract


