Oligometastatic disease usually includes a limited number of lesions (≤5),1 and includes several disease settings, with de-novo oligometastatic state (oligometastatic at the time of diagnosis), repeat (patients with a previous history of oligometastatic disease) and induced oligometastatic disease (previous history of polymetastatic disease).2 There is now growing evidence that patients with CRPC may derive benefit from SBRT in oligoprogressive or oligometastatic disease, with the potential for improvement in outcomes and quality of life. However, except for a few prospective trials, most evidence remains retrospective.
Metachronous oligoprogression is defined as an oligometastatic disease (≤5 lesions) diagnosed in a patient with recurrent metastatic disease, under active systemic treatment at the time of diagnosis of oligometastases, and with no previous history of oligometastatic disease (Figure 1A).2 In this population of patients, Francolini et al. recently reported the outcomes of men treated within the ARTO randomized phase II trial, assessing the impact of the addition of SBRT to acetate abiraterone and prednisone (AAP), in patients with non-visceral oligometastatic CRPC.3 The primary endpoint was the biochemical response (BR), defined as a prostate-specific antigen (PSA) decreased ≥50% from baseline measured at 6 months from treatment start. BR was detected in 68.8% and 92% of men receiving AAP and AAP + SBRT, respectively. Addition of SBRT to AAP enabled a significant improvement in progression-free survival (PFS) (hazard ratio of 0.35, p<0.001). Though the study was not powered to determine the impact of such strategies on OS, hazard ratio (HR) for death favored the AAP + SBRT arm but remained non-significant (HR= 0.35 [95% CI: 0.28 – 1.49]). In patients continuing androgen deprivation therapy (ADT) alone, the biochemical progression-free survival (bPFS) ranged between 9.5 months 17.9 months, and 5, and the next systemic treatment-free survival (NEST-FS) reached up to 2 years.6
Induced oligoprogression is defined as the appearance of an oligoprogressive disease in patients with a previous history of polymetastatic disease and currently under active treatment (Figure 1B).2 In this population of patients, the recently published MEDCARE trial reported a median next systemic treatment-free survival (NEST-FS) reaching 17 months. In other trials, NEST-FS was reported to reach up to 3 years.7 Overall, SBRT was well tolerated, with less than 5% grade 3 toxicity reported across studies.
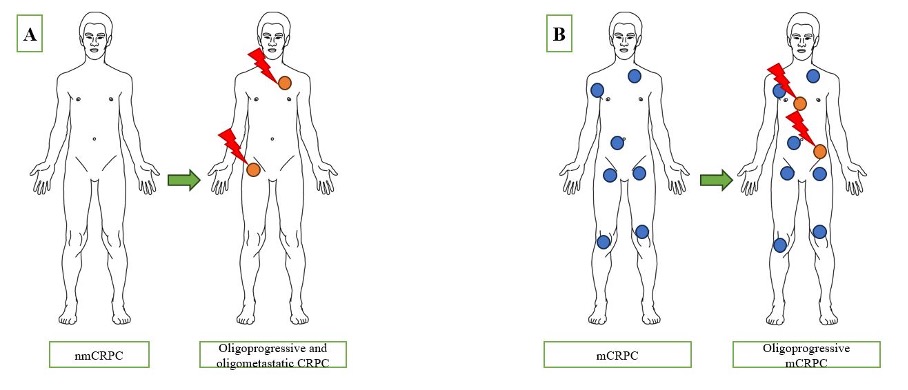
Figure 1: Implementation of SBRT for Oligo-Progressive CRPC. Legend: Red Arrow: Conduction of SBRT, Orange: Oligoprogressive Sites
A: Situation of metachronous oligoprogression, defined as an oligometastatic disease (≤5 lesions) diagnosed in a patient with recurrent metastatic disease, under active systemic treatment at the time of diagnosis of oligometastases, and with no previous history of oligometastatic disease
B: Situation of induced oligoprogression, defined as the appearance of an oligoprogressive disease in patients with a previous history of polymetastatic disease and currently under active treatment
The question of performing SBRT with continuation or change of systemic therapy for oligoprogressive CRPC patients remains to date open. In 2024, 45% of the experts from the Advanced Prostate Cancer Consensus Conference (APCCC) voted in favor of a switch of systemic therapy and SBRT in metachronous oligoprogressive CRPC. In men with induced oligoprogression, 49% of the experts voted in favor of SBRT and continuation of the same systemic therapy. No consensus was found for any of the proposed options. While explorative analysis suggests that in men with induced oligoprogression, SBRT combined with a change of systemic therapy might improve oncological outcomes beyond NEST-FS, this question will have to be answered in future prospective trials.8
To conclude, in the population of patients with oligometastatic CRPC, SBRT enables long-term biochemical response and PFS. In the oligoprogressive setting, SBRT could be integrated to prolong the duration and efficacy of systemic therapies. Nevertheless, the level of evidence remains very low, and inclusion within prospective trials remains the preferred option for this population of patients.
Written by: Jennifer Le Guevelou,1 Francesco Cuccia,2 Ronan Flippot,3 Giuseppe Ferrera,2 Mario Terlizzi,4 Thomas Zilli,5-7 Renaud De Crevoisier,8 Jean-Michel Hannoun-Levi,9 Stephane Supiot,10 Paul Sargos,11 David Pasquier,12,13
- Department of Radiation Therapy, Centre Eugène Marquis, Rennes, France.
- Department of Radiation Therapy, ARNAS Civico Palermo, Palermo, Italy.
- Department of Medical Oncology, Institut Gustave Roussy, Villejuif, France.
- Department of Radiation Therapy, Institut Gustave Roussy, Villejuif, France.
- Department of Radiation Oncology, Oncology Institute of Southern Switzerland, EOC, Bellinzona, Switzerland.
- Università della Svizzera Italiana, Lugano, Switzerland.
- Faculty of Medicine, University of Geneva, Geneva, Switzerland.
- Department of Radiation Therapy, Centre Eugène Marquis, Rennes, France.
- Department of Radiation Oncology, Centre Antoine Lacassagne, University Côte d'Azur, Nice, France.
- Department of Radiation Oncology, Institut de Cancérologie de l'Ouest, Nantes, France.
- Department of Radiation Oncology, Institut Bergonié, Bordeaux, France.
- Academic Department of Radiation Oncology, Centre Oscar Lambret, Lille, France.
- Lille University, CRIStAL UMR CNRS 9189, Lille, France.
References:
- Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radiation oncology perspective: An ESTRO-ASTRO consensus document. Radiotherapy and Oncology 2020;148:157–66.
- Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, deSouza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. The Lancet Oncology 2020;21:e18–28.
- Francolini G, Allegra AG, Detti B, Di Cataldo V, Caini S, Bruni A, et al. Stereotactic Body Radiation Therapy and Abiraterone Acetate for Patients Affected by Oligometastatic Castrate-Resistant Prostate Cancer: A Randomized Phase II Trial (ARTO). JCO 2023;41:5561–8.
- Zhang H, Orme JJ, Abraha F, Stish BJ, Lowe VJ, Lucien F, et al. Phase II Evaluation of Stereotactic Ablative Radiotherapy (SABR) and Immunity in 11C-Choline-PET/CT–Identified Oligometastatic Castration-Resistant Prostate Cancer. Clinical Cancer Research 2021;27:6376–83.
- Lohaus F, Zöphel K, Löck S, Wirth M, Kotzerke J, Krause M, et al. Can Local Ablative Radiotherapy Revert Castration-resistant Prostate Cancer to an Earlier Stage of Disease? European Urology 2019;75:548–51.
- Onal C, Kose F, Ozyigit G, Aksoy S, Oymak E, Muallaoglu S, et al. Stereotactic body radiotherapy for oligoprogressive lesions in metastatic castration-resistant prostate cancer patients during abiraterone/enzalutamide treatment. Prostate 2021;81:543–52.
- La Vecchia M, Fazio I, Borsellino N, Lo Casto A, Galanti D. Stereotactic body radiotherapy in oligoprogressive metastatic castration-resistant prostate cancer during abiraterone or enzalutamide. Tumori 2023;109:413–7.
- Deek MP, Taparra K, Phillips R, Velho PI, Gao RW, Deville C, et al. Metastasis-directed Therapy Prolongs Efficacy of Systemic Therapy and Improves Clinical Outcomes in Oligoprogressive Castration-resistant Prostate Cancer. European Urology Oncology 2021;4:447–55.


