Integrating Patient-Reported Outcomes Measures [PROMs] and Patient-Reported Experience Measures [PREMs] in preoperative shared decision-making is nowadays an unmet clinical need, to inform on the benefit-risk assessment of different PCa treatments.
This systematic review aimed to report and compare PROMs and PREMs after all recommended treatments for localized PCa (RP, RT, AS), as well as to provide a contemporary state of the art of which PROMs and PREMs are currently used within PCa settings.
1. Evidence Acquisition
A literature search was performed using the MEDLINE, EMBASE, and Cochrane CENTRAL databases, following the EAU Guidelines Office and the PRISMA statement recommendations.
The protocol has been registered in the International Prospective Register of Systematic Reviews database (PROSPERO: CRD42023485528).
The PICOS (Patient, Intervention, Comparison, Outcome, Study type) model was used to frame and answer the clinical question:
- P: Adult (> 18 years old) male patients with localized PCa, who had not undergone any previous treatment prior to their primary treatment for PCa;
- I: Active management for PCa according to EAU Guidelines recommendations. In particular, management options include: AS, RP (by any approach) or RT (including both EBRT and Low-Dose Rate [LDR] or High-Dose Rate [HDR] BT, with or without neoadjuvant/concurrent/adjuvant ADT);
- C: RP vs. RT (EBRT or BT) vs. AS (all management options should have been included in the study)
- O: PROMs and/or PREMs on urinary function and continence, bowel and sexual function, and Quality of Life [QoL];
- S: Prospective randomized and non-randomized studies.
Risk of bias was assessed using the Cochrane Handbook for Systematic Reviews of Interventions risk-of-bias tool for RCTs, and the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool for prospective studies.
Given the quality of the evidence retrieved, a quantitative synthesis/meta-analysis of the included studies was not feasible. As such, a narrative synthesis was used to summarize the review findings.
2. Evidence synthesis
The literature search identified 2564 papers, of which 21 were considered for the results and analyzed. Among the 21 papers included in this review, 1 reported data from a RCT (ProtecT trial), 12 were prospective non-randomized longitudinal studies, 3 were population‐based prospective studies, and 5 were cross-sectional studies.
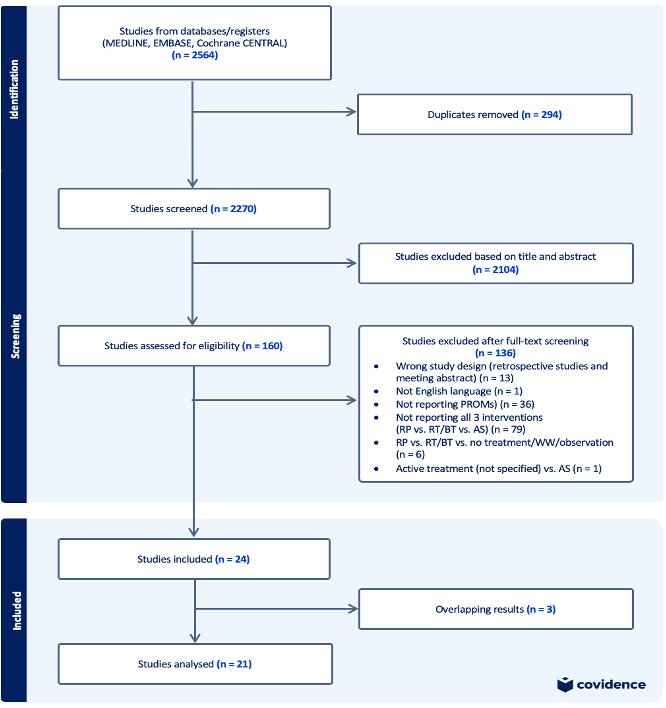
Figure 1. Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) Flowchart
2.1. PROMs for urinary function
Several authors reported an improvement of obstructive symptoms after RP, while up to 30-60% of patients treated with RT (mostly BT) report acute voiding and storage symptoms, with resolution over 1 to 2 years to levels similar to baseline.
2.2 PROMs for urinary incontinence
All studies included consistently show how RP leads to a greater adverse effect on continence compared to RT and AS, especially in the early period after treatment (up to 60-70% of patients reported to use pads at 2 months after surgery), with a sudden improvement over time (up to 20% by 2 years). Conversely, pad use after EBRT and BT was stable during follow-up, with about 5% of patients reporting UI at 2 years.
2.3 PROMs for sexual function
Sexual function was the most impaired functional domain, with RP showing the highest impact (up to 80-90% of patients reported erectile dysfunction after surgery, decreasing to approximately 60% by 2 years). As expected, AS showed a minor effect on erectile function, although a steady decline in sexual functioning was largely reported. This constant and progressive decline confirms that not only the type of treatment received, but also aging and other factors are implicated in the genesis of erectile dysfunction.
2.4 PROMs for bowel function
There is no consensus on the effect of different treatments on bowel function, since only a small part of the studies found significant difference. Nevertheless, a worsening of bowel function was mainly observed in the population treated with RT (15-40% of patients reporting acute bowel bothers after radiation, with subsequent better recovery for patients treated with BT than with EBRT. No significative differences were assessed considering RP or AS.
2.5 PROMs for QoL
A heterogeneous variety of PROMs has been used to assess QoL. Most of them found no significant difference among all treatment groups (except for worst QoL scores in patients receiving hormonal therapy or chemotherapy).
2.6 PREMs after active surveillance vs radiation therapy vs radical prostatectomy
Only 3 prospective observational studies reported PREMs. Decision-regret was reported to be relatively frequent among patients experiencing unwanted physical, psychosocial, and oncological outcomes, irrespectively of the treatment modality (up to 23% of the patients).

Figure 2. Effect of Treatments on Functional Domains and Quality of Life
Conclusions: All recommended treatments for localized PCa have an impact on PROMs and PREMs, yet on different domains and with different severities. Our findings reveal that RP mostly affects urinary continence and sexual function, with better results on voiding symptoms compared to other treatments. Bowel function and voiding symptoms are more impaired by RT. None of the treatments showed a significant impact on mental or physical QoL.
Only a few studies reported PREMs, highlighting the unmet need to explore these outcomes in future studies. These papers showed a non-negligible proportion of patients reporting decisional regret, irrespectively of the treatment modality.
These findings support the need to set realistic expectations when counseling patients with localized PCa, individualizing the approach to the patient. Moreover, standardization of PROMs collection in real-world practice and clinical trials is urgently warranted.
Written by: Andrea Alberti,1,2 Rossella Nicoletti,1,2,3 Daniele Castellani,4 Yuhong Yuan,5 Martina Maggi,6 Edoardo Dibilio,1,2 Giulio Raffaele Resta,1,2 Pantelis Makrides,1,2 Francesco Sessa,1,2 Arcangelo Sebastianelli,1,2 Sergio Serni,1,2 Mauro Gacci,1,2 Cosimo De Nunzio,7 Jeremy Yuen Chun Teoh,3,8 Riccardo Campi1,2
- Unit of Urological Robotic Surgery and Renal Transplantation, University of Florence, Careggi Hospital, Florence, Italy
- Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy.
- S.H.Ho Urology Centre, Department of Surgery, The Chinese University of Hong Kong, Hong Kong, China
- Urology Unit, Azienda Ospedaliero-Universitaria delle Marche, Università Politecnica delle Marche, Ancona, Italy
- Department of Medicine, McMaster University, Hamilton, Ontario, Canada
- Department of Urology, Sapienza Rome University, Rome, Italy
- Department of Urology, Sant’Andrea Hospital, La Sapienza University, Rome, Italy
- Department of Urology, Comprehensive Cancer Center, Medical University of Vienna, Vienna, Austria.


