However, MRI misses many cancers. Comparisons of mpMR images to whole mount surgical pathology found that 35% of individual GG ≥ 2 PCa lesions were missed on MRI. The rate was considerably higher for lesions < 1 cm2. Systematic reviews report that systematic biopsies identified GG ≥ 2 prostate cancer in 15% of cases where targeted biopsies were negative.
Concern regarding invisible cancers has driven many interventions. This concern drives systematic biopsies in men with targeted biopsies and drives systematic biopsies in men with negative imaging. It undermines the appeal of focal therapy because of concerns about missed, untreated cancers, and foments anxiety in patients undergoing active surveillance.
Recent radiogenomic studies have demonstrated that the genetic aberrations that account for tumor visibility on MRI are the same mutations that underlie cancer invasion and metastasis. The implication is that invisible cancers, even if histologically ‘significant’, are both genomically indolent and benign in their behavior. The radiogenomic data is now supported by several clinical studies in men on active surveillance, which report that MR invisibility is a powerful predictor for an exceedingly low rate of progression to higher grade cancer. A large radical prostatectomy series stratifying patients by MR invisibility vs visibility found that the MR invisible cancers had negligible rates of biochemical relapse, progression, or metastasis.
In this manuscript, to address the question of the clinical significance of MR invisibility, we compared the natural history of MR visible vs invisible cancers in men on active surveillance. MRI was formally incorporated into our AS protocol in 2013. We included patients who were diagnosed prior to 2013 and had an MRI within 2 years of diagnosis.
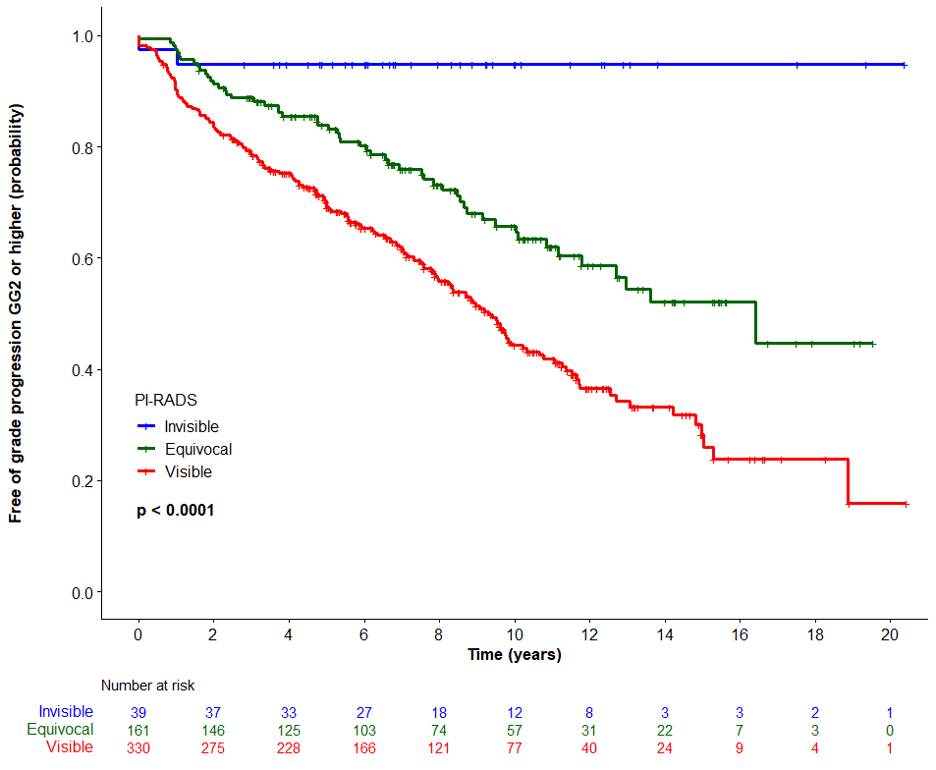
530 AS patients had one or more MRIs, with a median follow up of 8.5 years. At baseline, 39 patients (7.4%) had negative MRIs (PiRADS 1-2), 161 (30%) equivocal (PiRADS 3), and 330 (62%) positive MRIs (PiRADS 4-5). 229 patients were upgraded; 5% of those with MR invisible lesions, 34% with PiRADS 3, and 52% with PiRADS 4-5 (Fig 1). 229 (43%) of the 530 men were eventually treated. No patient with PiRADS 1-2 at baseline required treatment, vs 36% with PiRADS 3 and 52% with PiRADS 4-5 (p<.001).
Kaplan Meier of time to grade progression by PiRADS baseline score:
The major limitation of this study was that men with invisible cancers had a lower rate of subsequent biopsies, raising the risk of ascertainment bias. However, we believe that given the long follow up (median 8.5 years), clinically significant invisible cancers would in most cases have manifested themselves during the prolonged follow up, which included serial imaging and PSA.
The inference is that invisible cancers are clinically insignificant in most cases. Thus they need not be sought after with systematic biopsies. This has significant implications for the requirement for systematic biopsies in the active surveillance setting. Dropping the need for systematic biopsies in these men has significant benefits in terms of inconvenience, discomfort, cost, co-morbidity, and the appeal of active surveillance as a management strategy.
Outliers exist. In this case, the outliers represent men with small high grade cancers, too early to be visible on MRI despite the adverse genomics. Clearly, ongoing follow up with periodic imaging and biopsy as indicated is mandated in these men. Based on radiogenomic and clinical data, it is predictable that these cancers will become visible over time, and diagnosed at a point where they are still curable. We emphasize that in our surveillance series, only 5% of the men with invisible cancers had grade progression, and none required treatment. Hence It appears the scenario of invisible missed cancers progressing to incurable disease is extremely uncommon. Further longitudinal studies are warranted to confirm this.
Written by: Laurence Klotz, CM, MD, FRCSC, Professor of Surgery, University of Toronto, Sunnybrook Chair of Prostate Cancer Research, Division of Urology, Sunnybrook Health Sciences Centre, Toronto, Ontario
Reference:
Read the Abstract


