BERKELEY, CA (UroToday.com) - Purpose: To assess the predictors of acute bowel toxicity after whole-pelvis irradiation (WPRT) and image-guided Tomotherapy with a simultaneous, integrated boost on the prostate/prostate bed.
Methods and Materials: In the period between March 2005 to April 2009, 178 consecutive patients with clinically localized prostate cancer underwent WPRT during radical (n = 77) or postoperative (n = 101) radiotherapy.
The main clinical characteristics of the population were the following: a median age of 71 years (range 45 to 89), 11% of patients suffered from diabetes, 39% suffered from hypertension, 39% had undergone previous abdominal/pelvic surgery, and 73% received some type of hormonal therapy before Tomotherapy. According to internal guidelines, WPRT was always prescribed: 1) in intermediate and high-risk groups of patients in a radical setting, 2) in node-positive patients and in node-negative patients submitted to a limited lymphadenectomy (< 8 removed nodes), 3) and/or in the presence of adverse prognostic factors (Gleason Score > 7 and/or preoperative PSA > 10 ng/mL) in an adjuvant or salvage setting.
All patients treated with radical intent and still potent underwent an MRI scan immediately after a CT scan to better define the prostate apex. Concerning the contouring of the pelvic nodes, the obturator, hypogastric, external and internal iliac, and presacral lymph nodes anterior to the first sacral segment were always included (CTVN) and drawn according to published guidelines [1,2].
Regarding organs at risk (OAR), the rectum (from the anus to the curvature in the sigmoid), bladder, femoral heads and femurs, bulb of the penis (in young and/or potent patients), and intestinal cavity (IC) outside the PTVs were contoured. IC was drawn starting from 1 cm above the cranial limit of PTV1 up to its caudal limit, including the sigmoid. Two well-skilled physicians contoured the bowel loops, and the cranial limit was put in coincidence with the limit of PTVN.
PTVN was obtained by isotropically expanding the CTVN by a 7 mm margin, while the remaining PTVs were obtained by expanding the respective CTVs by 8 mm in the left/right and anterior/posterior directions, and by 10 mm in the cranial/caudal one.
WPRT was delivered with Helical Tomotherapy, with a moderately hypofractionated (28 fractions; median duration 42 days) regimen, prescribing the following doses: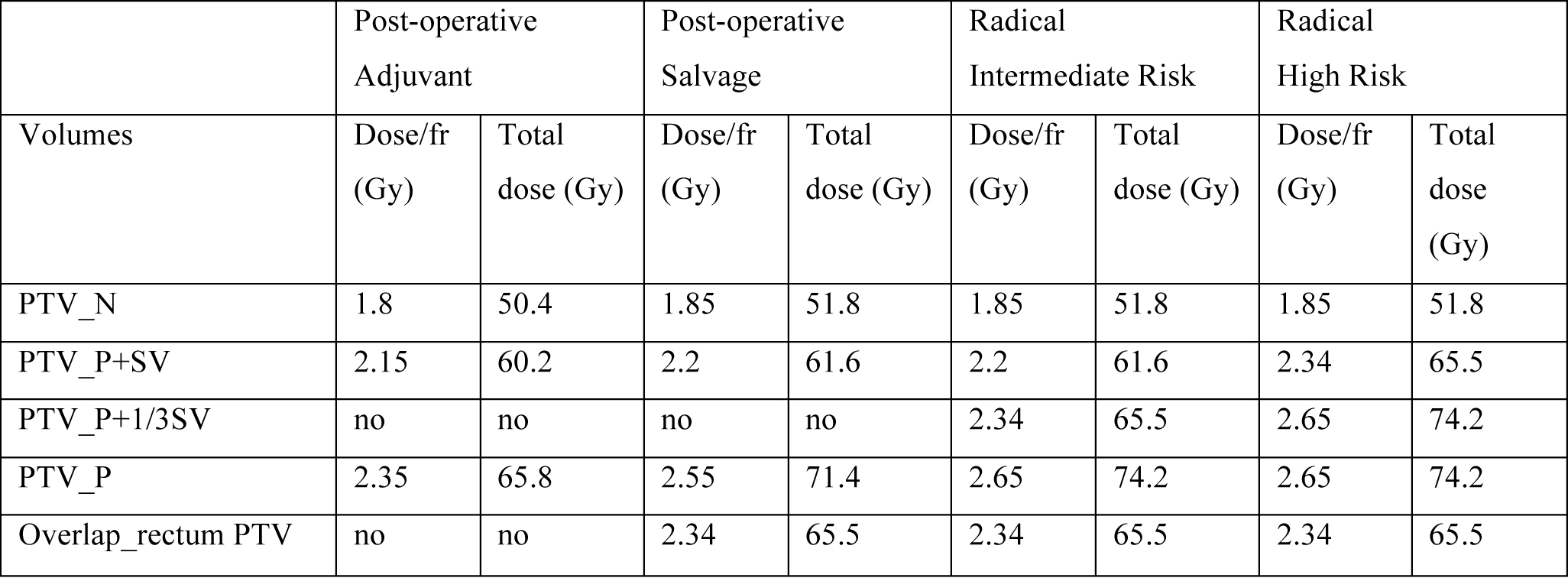
Concomitant to pelvis irradiation, different doses were delivered to seminal vesicles (SV), third proximal vesicles (1/3SV), and the prostatic bed or prostate (P), always in 28 fractions.
Concerning planning optimization strategies for the rectum, bladder, and IC, after satisfying constraints regarding the “high” doses (for rectum: V65 < 15%, V70 < 1%; for bladder: Dmax < 105%; for IC: Dmax < 55 Gy, V50 < 55 Gy and V50 < 55 Gy and V50 [3,4] outside PTVs (not only the loops). Concerning femoral heads, the constraints were: < 55 Gy and V50 < 2%.
The ratio between loop volume and PTVN volume (RLPTVN) roughly represents the “density” of loops in the fraction of IC irradiated. The impact of many anatomical and clinical parameters on >grade II, acute bowel toxicity was investigated by logistic analyses.
Results: Only 15/178 patients (8.4%) experienced grade II toxicity (zero grade III). The main predictors during univariate analysis were nodal CTV (CTVN > 380 cc, OR: 3.7, p = 0.017), treatment duration (< 40 days, OR: 6.2, p = 0.006), and grade II, acute rectal toxicity (OR: 6.5, p = 0.015). CTVN correlated with acute, upper gastrointestinal toxicity. A multivariate analysis, including only pretreatment variables, revealed an independent role of CTVN and age. If we included treatment-related factors, the best predictors were age (> 66 years), treatment duration (< 40 days), and grade II rectal toxicity. This last correlated with the overlap between PTVN and loops (OVPN > 51 cc, OR: 14.4, p = 0.0003) that is representative of the volume of loops receiving the prescribed dose (51.8 Gy, 1.85 Gy/fr).
Conclusions: Acute bowel toxicity after WPRT Tomotherapy is mild, relatively rare, and associated with larger CTVN and older age. While efforts to further reduce it do not appear to be relevant, the pretreatment assessment of "high-risk" patients may help physicians to better manage symptoms. A prospective validation would be very important in confirming these results and in refining dose-volume bowel effects, including symptoms milder that the ones investigated and retrospectively assessed here.
References:
- Lawton CA, Michalski J, El-Naqa I, et al. RTOG GU Radiation oncology specialists reach consensus on pelvic lymph node volumes for high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2009;74:383-387.
- Martinez-Monge R, Fernandes PS, Gupta N, Gahbauer R. Cross-sectional nodal atlas: a tool for the definition of clinical target volumes in three-dimensional radiation therapy planning. Radiology. 1999;211:815-828.
- Fiorino C, Alongi F, Perna L, et al. Dose-volume relationships for acute bowel toxicity for patients treated with pelvic nodal irradiation for prostate cancer. Int J Radiat Oncol Biol Phys. 2009;75:29-35.
- Sanguineti G, Little M, Endres EJ, et al. Comparison of three strategies to delineate the bowel for whole pelvis IMRT of prostate cancer. Radiother Oncol. 2008;88:95-101.
Written by:
Fiorino C, MD., Et Al., as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.



