BERKELEY, CA (UroToday.com) - PSA screening reduces prostate cancer mortality.[1, 2] Therefore, general practitioners and urologists are increasingly confronted with requests for PSA testing. However, there are several substantial harms as a result of screening, such as unnecessary biopsies and over-diagnosis. Furthermore, there is uncertainty surrounding the follow-up of men who were screened negatively for prostate cancer. When the screening test or the prostate biopsy is negative, physicians often struggle with questions regarding if and how to continue testing.
To provide support in these difficult decision points, we have developed the future-risk calculator, based on data from 15 791 screen-negative men at the initial screening round from the Rotterdam branch of the ERPSC trial.[3] This calculator is readily available on our website: www.prostatecancer-riskcalculator.com. It was based on initial screening data on age, PSA, digital rectal examination, family history, prostate volume, and information on previous biopsy. The outcome was the 4-year risk of biopsy-detectable prostate cancer, which was a priori categorized as no cancer, cancer with a low risk of progression, and cancer with a potentially high risk of progression. The 4-year predictions were validated with additional follow-up data up to 8 years after initial screening.
We have found that positive family history, and especially PSA level, predicted prostate cancer, whereas a previous negative biopsy or a large prostate volume reduced the likelihood of future cancer. For illustration, Figure 1A depicts the predictions for a 65-year-old man with a PSA of 2.5 ng/ml and a prostate volume class of 40 cm3. If all the other predictors are set on zero, the 4-year risks of low-risk cancer and high-risk cancer are 5.5% and 1.7%, respectively. An abnormal digital rectal examination outcome and a positive family history (Figure 1B) would increase this man’s risk for high-risk cancer to 4.2%. If this man had already had a prostate biopsy with a benign result at initial screening (i.e., initially no cancer detected), his future risk of having prostate cancer would decrease to 3.3% (2.0% for low-risk cancer and 1.3% for high-risk cancer) (Figure 1C). Additional 8-year follow-up data confirmed the predictions.
In addition, we have proposed a stratification of future risk into low (≤ 1.0%), moderate (1.0–5.0%), and elevated risk (≥ 5.0%), based on the mean and median future risks of having prostate cancer (Table 1). We suggest that men with a low predicted 4-year risk (≤ 1.0%) could be rescreened at longer intervals, or not at all, depending on competing risks, while men with an elevated 4-year risk (≥ 5%) could be advised that they are at increased risk for prostate cancer, and might benefit from immediate retesting.
It should be acknowledged that this newly developed risk calculator needs external validation to confirm its results and to evaluate its applicability in other cohorts. Because of differences in the patterns of early detection, the value of nomograms outside of the model populations may not be the same. The calculator may underestimate or overestimate risks based on the characteristics of the study cohort, such as age, ethnicity, number of previous PSA tests, template of the biopsy performed, and number of previous negative biopsies.
External validation of the future risk calculator may, however, not be that easy, as it requires up to 4 years of follow-up data to verify the outcomes. Until this has been realized, we might rely on the previous promising results of the calculators based on the ERSPC; several studies have shown adequate discrimination and calibration of these prediction models in contemporary, independent cohorts.[4, 5]
A growing body of evidence has suggested that shared-decision making is warranted to maximize the benefits of screening and minimize its harms.[6, 7] In that context, the future risk calculator may be a promising tool for reducing uncertainty, unnecessary testing, and over diagnosis of prostate cancer.
Figure 1A: 4-year future risk of a 65-year-old man, PSA 2.5 ng/ml, normal DRE, no family history, prostate volume class of 40 cm3, and no previous biopsy.
Figure 1B: 4-year future risk of a 65-year-old man, PSA 2.5 ng/ml, abnormal DRE, positive family history, prostate volume class of 40 cm3, and no previous biopsy.
Figure 1C: 4-year future risk of a 65-year-old man, PSA 2.5 ng/ml, abnormal DRE, positive family history, prostate volume class of 40 cm3, and having had a previous negative biopsy.
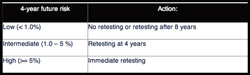
Table 1: A possible future risk-based screening algorithm
References:
- Schroder FH, Hugosson J, Roobol MJ, et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 2012;366:981-90.
- Hugosson J, Carlsson S, Aus G, et al. Mortality results from the Goteborg randomised population-based prostate-cancer screening trial. Lancet Oncol 2010;11:725-32.
- Roobol MJ, Zhu X, Schroder FH, et al. A Calculator for Prostate Cancer Risk 4 Years After an Initially Negative Screen: Findings from ERSPC Rotterdam. Eur Urol 2012;
- Trottier G, Roobol MJ, Lawrentschuk N, et al. Comparison of risk calculators from the Prostate Cancer Prevention Trial and the European Randomized Study of Screening for Prostate Cancer in a contemporary Canadian cohort. BJU Int 2011;108:E237-44.
- van Vugt HA, Roobol MJ, Kranse R, et al. Prediction of prostate cancer in unscreened men: external validation of a risk calculator. Eur J Cancer 2011;47:903-9.
- Roobol MJ, Steyerberg EW, Kranse R, et al. A risk-based strategy improves prostate-specific antigen-driven detection of prostate cancer. Eur Urol 2010;57:79-85.
- Zhu X, Albertsen PC, Andriole GL, Roobol MJ, Schroder FH, Vickers AJ. Risk-based prostate cancer screening. Eur Urol 2012;61:652-61.
Written by:
Xiaoye Zhu, MD* and Monique J. Roobol, PhD, MSc as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.
*Corresponding author:
Department of Urology Erasmus MC, University Medical Center Rotterdam
Room NH-227
P.O. Box 2040
3000 CA Rotterdam
The Netherlands

More Information about Beyond the Abstract


