BERKELEY, CA (UroToday.com) - Androgen deprivation therapy (ADT) is commonly used as an adjunct to curative radiation therapy for prostate cancer (PC), or as primary treatment for advanced or metastatic PC. However, ADT comes with costs in terms of adverse events and financial burden. The most concerning associated adverse events include decrease in bone mineral density with potential risk of fracture, a metabolic syndrome (increased cholesterol, triglycerides, and insulin resistance), diabetes, and possibly myocardial infarction. ADT is costly, and many patients are treated for years. The additional costs for monitoring and treating adverse events are largely unknown.
The purpose of this study was to estimate total health care costs among PC patients receiving ADT in the province of Ontario, Canada, and to quantify the additional costs associated with ADT’s frequently documented, serious, and potentially costly adverse events.
We used the Ontario Cancer Registry and health care administrative data to identify all PC patients (ICD-9-CM 185) in Ontario, Canada who started ≥90 days of ADT or had orchiectomy at age ≥66 in 1995-2005 (n=26,809). The diagnosis dates of adverse events before and after ADT initiation were determined from administrative data: myocardial infarction (MI), acute coronary syndrome, congestive heart failure, stroke, deep vein thrombosis/pulmonary embolism, any diabetes, and fracture/osteoporosis. We excluded patients with the same diagnosis pre-ADT as post-ADT and allocated each patient’s time from ADT initiation (index date) to death or December 31, 2007 into health states: ADT (no adverse event), ADT_AE (specified single adverse event), Multiple (>1 event), and Final (≤180 days before death). We estimated annual total health care costs during each state using methods for Canadian health administrative data.
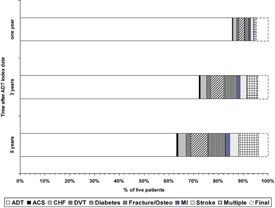 |
| Figure 1. |
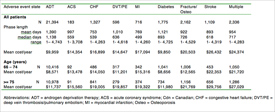 |
| Table 1. Patients, duration, and total costs ($2009 Cdn) for ADT and adverse event health states for patients with a new post-ADT adverse event |
Figure 1 shows the proportion of patients in each health state (ADT with no adverse event, an adverse event, or final) at one, three, and five years after their Index dates, excluding patients who died (7%, 30%, and 50% of the entire cohort at one, three, and five years, respectively). After one year of ADT, 9.5% of the surviving patients were in an adverse event health state. Over time, patients moved from ADT into adverse event states or died. Five years after initiating ADT, the most common adverse event states were diabetes and stroke.
Table 1 shows the allocation of patients’ observation time to health states, after excluding patients who had the same adverse event before and after ADT. Almost all patients (98%) had time in the ADT state. Approximately 37% of patients (N=8,095) were in at least one adverse event state. Diabetes was the most common and longest adverse event state (n=1,775; mean duration=1,120 days). The table also shows the mean annual cost for each state. The costliest adverse event state was stroke ($26,432/year). Multiple was the most frequently experienced (n=2,336) and second most costly ($24,374/year). Costs for all adverse event health states increased with age. Changes in costs across comorbidity strata were smaller and less consistent (data not shown).
Our study is, to our knowledge, the only economic analysis that included seven adverse events that have been associated with ADT. We found that managing adverse events adds a considerable economic burden to the care of patients receiving ADT.
We cannot say that the frequencies of these conditions are greater with ADT than they would have been without in this patient population. Likewise, we did not attempt to attribute costs to the adverse events. Many health care services included on the data could have been related to PC or other health problems, while others were likely treating PC. We did not estimate total health care costs in PC patients who did not receive ADT because finding adequately matched non-ADT PC patients in the real world would be difficult; ADT is recommended for certain types of PC, and patients who receive ADT differ in age and comorbidity from PC patients who receive other treatments. We provided accurate estimates of the total cost profiles of PC patients who experienced adverse events that have been documented as common ADT complications, including trends across age and comorbidity. These data can inform pharmaco-economic and cost-effectiveness models, which are typically state-transition models incorporating health states such as those defined in our study.
Clinical practice guidelines and reimbursement recommendations should consider the health care costs related to adverse events that may be associated with ADT in the risk/benefit calculation of treatment.
Written by:
Karen E. Bremner, BSc as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.
Toronto General Research Institute, Toronto General Hospital, Toronto, ON Canada

More Information about Beyond the Abstract


