Patients with chronic renal injury are generally at higher risk for severe COVID-19 infections. However, this review noted one study by Bastile et al which showed that patients on hemodialysis with COVID-19 had less lymphopenia, lower serum levels of inflammatory cytokines, and milder clinical disease compared to other COVID-19 patients. Dialysis patients are recommended to continue their current regimen and stay at their current center to minimize exposure risk. Not surprisingly, patients without pre-existing kidney disease were at higher risk of developing acute kidney injury after becoming infected with SARS-CoV-2. Elevated baseline serum creatinine, elevated baseline BUN, AKI stage, proteinuria, and hematuria were all found to be independent risk factors for in-hospital death. Patients that underwent computed tomography (CT) scans of kidneys were also more likely to have reduced density, suggestive of inflammation. As schematically illustrated in Figure 1, the effects of the viral interaction with ACE2 can cause kidney damage through a heightened inflammatory response.
Immune checkpoint inhibitors (ICIs) have played a major role in the treatment of advanced RCC and also likely modulate the cytokine release and contribute to the severity of COVID-19. Further, COVID-19 related interstitial pneumonia could be worsened by potential pulmonary toxicity from anti-PD-1/PD-LI ICI agents. At this time, discontinuation of ongoing treatment with ICIs for patients is not recommended. There has been some evidence that tocilizumab, a monoclonal antibody against the interleukin-6 receptor may serve as a neutralizing antibody. ACE inhibition is typically used to treat hypertension but has a theoretical benefit for RCC as well. ACE inhibitors cause an increase in ACE2 receptors and less competitive inhibition for SARS-CoV-2 binding. By utilizing a different mechanism, endothelin receptor antagonists may be better suited for those with hypertension as it does not enhance the viral binding capability of SARS-CoV-2.
Kidney function and SARS-CoV-2 infectivity intimately overlap at the cellular and molecular level via signaling exchanges. As a result of these interactions, challenging clinical scenarios have arisen, particularly in patients with RCC and COVID-19. Joint decision making should be enacted to identify the best course of action for each patient. Targets for treating and aiming to cure COVID-19 are actively being pursued, though each is faced with some challenges. There is promise in the emerging evidence that the monoclonal antibody tocilizumab may be effective at neutralizing the virus. Others have sought to target SARS-CoV-2 RNA, though the viral RNA domains must first be identified and has limits of oligonucleotides being targeted only in the lungs. Current antivirals, such as those for HIV, are being tested. Remdesivir was clinically effective in the treatment of COVID-19 in one patient in the United States. Larger scale studies are required as we answer the call of our generation to provide a rigorous scientific evidence-based knowledge and implement therapeutic options to overcome COVID-19 globally.
Some evidence has emerged that convalescent plasma transfer from a previously recovered patient to an actively infected patient can increase the immune response against severe infections. This treatment strategy is largely limited by the speed of development. Targeting the ACE2 receptor itself is also under investigation. An in vitro study showed that an antibody targeting ACE2 successfully blocked SARS-CoV-2 entry into the host cell (Figure 1).
Undoubtedly, clinicians will continue to face difficult decisions for the best management for their patients while minimizing the risk of SARS-CoV-2 infection. ACE2 expression in the kidney, particularly in RCC, will allow for new insights into therapeutic targeting and treatment. Utilizing extracellular vesicles/exosomes cfDNA, CTCs, biomarkers, and the genomic landscape of RCC and COVID-19 positive patients will allow for further understanding of the effect of viral damage on kidney function and RCC. The scientific rationale built on molecular and biological knowledge of overlapping processes is a strong driver of future clinical work that can have immediate therapeutic benefit in the management of renal cancer patients diagnosed with COVID-19.
As the nation and humanity face a post-pandemic era, we join forces with other investigative teams to fight the war against the SARS-CoV-2 virus and cancer.
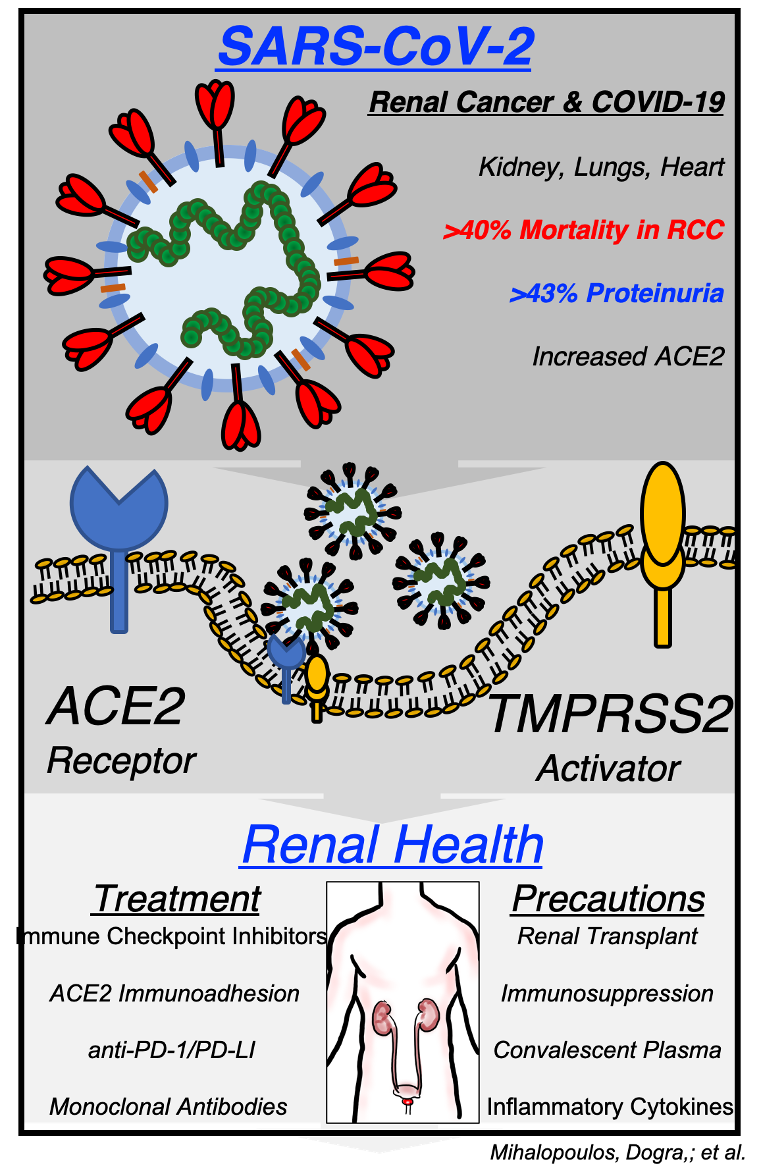
Figure 1. Molecular pathway of SARS-CoV-2 uptake by host cells and infection on renal disease with potential therapeutic targeting of RCC
Written by: Andrew Katims, MPH, MD, Navneet Dogra, PhD, Natasha Kyprianou, PhD, and Ketan Badani, MD, Departments of Urology, Pathology and Oncological Science, Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, New York
Read the Abstract


