Renal mass in a solitary kidney (RMSK) is a major challenge that has traditionally been managed with partial nephrectomy (PN) to avoid dialysis and achieve durable cancer-free status.1 However, is PN always possible, and how often can these goals be achieved?
Is radical nephrectomy (RN) ever required and why, and what other options can be considered for this patient population? How should patients with RMSK be evaluated? Unfortunately, the literature regarding RMSK has been limited in terms of numbers of patients under analysis and most studies have only reported patients for whom PN was achieved,2 thus not providing a full picture regarding the potential complexities of management.
To address this, we recently reviewed our experience with RMSK (1975-2022, n=1,066) with inclusion of all patients to provide a more comprehensive and informative analysis.3 Forty-eight patients with horseshoe kidneys were reported on separately,4 leaving 1,024 with RMSK in an orthotopic kidney. For these patients, median tumor size and R.E.N.A.L. score were 3.7 cm (IQR: 2.5-5.2 cm) and 8 (IQR: 6-10), respectively, and median follow-up was 53 months.
Overall, 842 (82%) patients were managed with PN. Of these, 95% were performed with vascular occlusion with median warm and cold ischemia times of 22 and 45 minutes, respectively. PN saved a mean of 82% of the global glomerular filtration rate (GFR) and dialysis-free survival for PN was 97% at 5 years, while 5 year recurrence-free survival was 83%. In the great majority of patients PN was thus able to provide strong oncologic and functional outcomes, but PN was not always possible. Forty-one patients had planned RN (4.0%), most often due to severe preexisting chronic kidney disease or inadequate parenchymal to be saved if PN was performed. In addition, 13 patients were converted from PN to RN (1.5%), most often due to concerns about surgical margins and oncologic control. With careful patient selection, 102 patients (10%) were managed with thermal ablation (TA) and 26 (3%) with active surveillance (AS).
Our study also confirmed substantial evolution in management with TA, AS, and minimally invasive PN (n= 86, 11%) only applied in the last 20-25 years. Since 2008, 22 patients (2.1% overall) with clear cell RCC and R.E.N.A.L. ≥ 10 (median=11) received neoadjuvant tyrosine kinase inhibitors to facilitate PN, leading to a 57% median decrease of tumor volume, and PN was accomplished in 20 (91%) of these patients. Ex-vivo surgery for RMSK at our center was abandoned in 1986 due to concerns about acute kidney injury and suboptimal functional outcomes; however, we recently performed ex-vivo PN for RMSK with venous involvement with strong functional results and uneventful recovery. Given this experience and technological advances, including fine vessel sealers and improved thrombogenic materials, this approach is now back in our armamentarium for RMSK.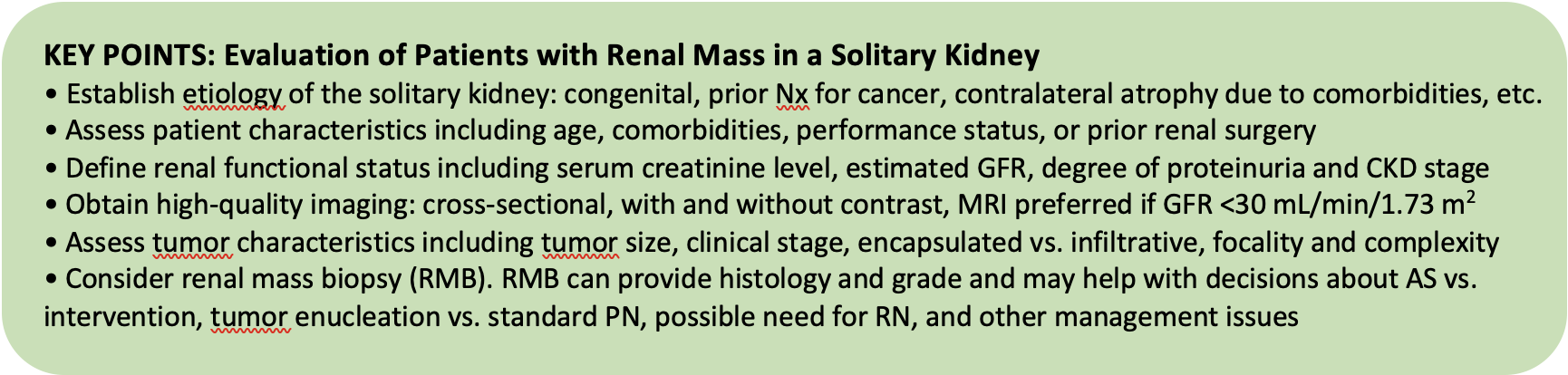
Table 1. Management of Patients with Renal Mass in a Solitary Kidney (RMSK). After defining patient, tumor, and functional considerations, patients with RMSK can be classified into one of five categories. Management options and priority are shown with focus on nephron-sparing approaches whenever possible.
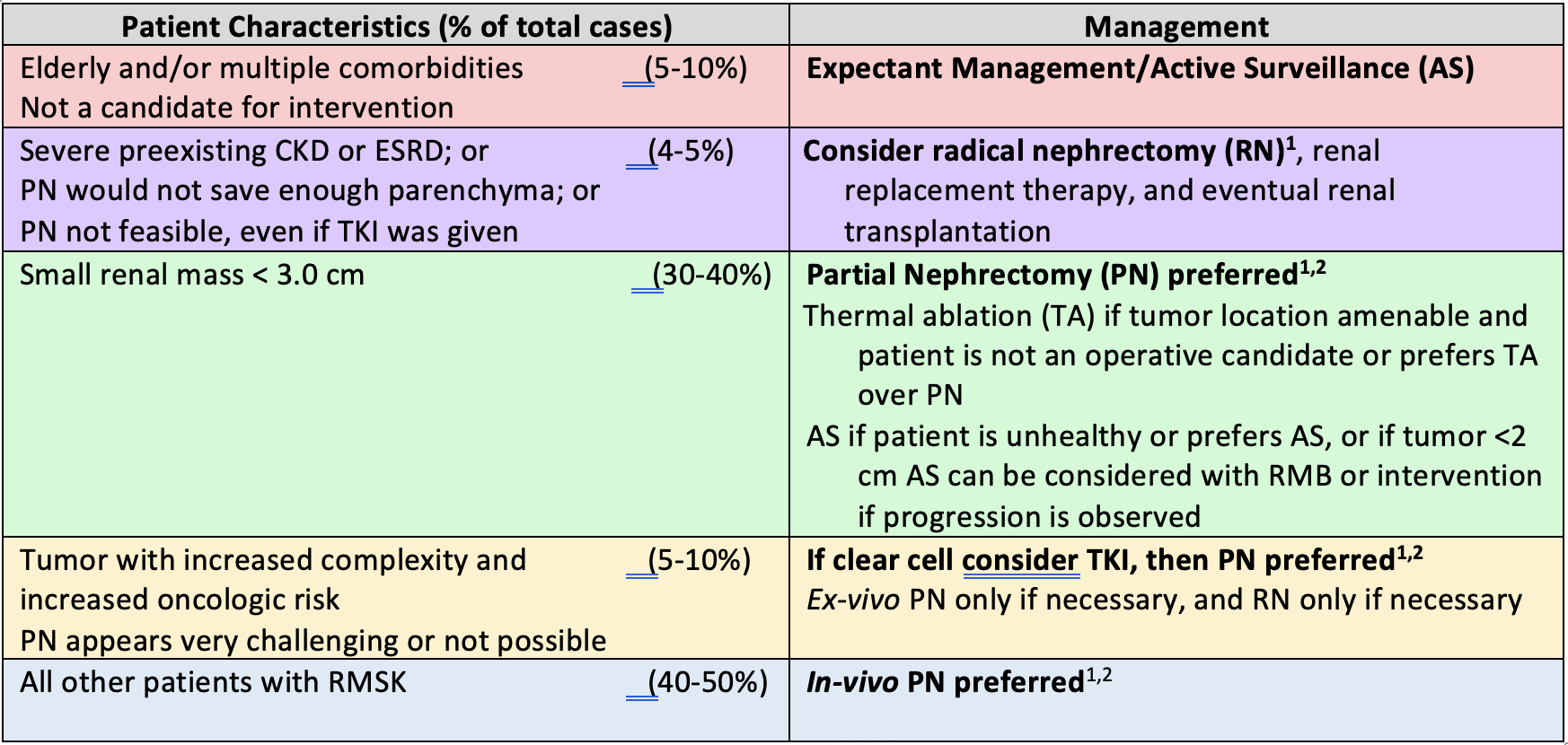
- Minimally invasive if possible.
- For PN, the main goal is to preserve as much vascularized renal parenchyma as possible and avoid prolonged warm ischemia. Options include clamped PN with hypothermia or limited warm ischemia, zero ischemia PN or ex-vivo PN with hypothermia.
Studies in progress are now looking in greater detail at short and long-term functional outcomes after PN for RMSK and the ultimate impact of tyrosine kinase inhibitors in patients with RMSK and high tumor complexity. A matched cohort study of TA versus PN for RMSK is also in progress.
Written by: Steven C. Campbell, MD, PhD, Professor of Surgery, Section of Urologic Oncology, Department of Urology, Glickman Urological and Kidney Institute, Cleveland Clinic
Co-Authors: Worapat Attawettayanon,1 Yosuke Yasuda,2 JJ Zhang,3 Carlos Munoz Lopez4
- Division of Urology, Department of Surgery, Faculty of Medicine, Songklanagarind Hospital, Prince of Songkla University, Songkhla, Thailand
- Tokyo Medical and Dental University, Graduate School, Tokyo, Japan
- Institute of Urologic Oncology, Department of Urology, University of California Los Angeles (UCLA), Los Angeles, CA
- Department of Urology and Lerner College of Medicine, Cleveland Clinic
- Campbell SC, Clark PE, Chang SS, et al: Renal mass and localized renal cancer: evaluation, management and follow-up: AUA Guideline part I. J Urol 2021;,206(2); 199-208.
- Fergany AF, Saad IR, Woo L, Novick AC. Open partial nephrectomy for tumor in a solitary kidney: experience with 400 cases. J Urol 2006; 175(5):1630-1633.
- Yasuda Y, Zhang JJH, Attawettayanon W, et al: Comprehensive Management of Renal Masses in Solitary Kidneys. Eur Urol Oncol 2023;6(1):84-94.
- Yasuda Y, Zhang JJ, Attawettayanon W, et al: Management of Renal Mass in Horseshoe Kidneys. Urology 2022;166:170-176.


