The first robotic RPLND (R-RPLND) was performed in 2006 by Davol and Rukstalis. The robotic approach has allowed greater dissemination due to several advantages of the robotic platform including enhanced vision with 3D optics, magnification, improved dexterity with the Endowrist of the DaVinci robotic platform, and ergonomic advantages for the surgeons that previously had to stand for 8-10 straight hours to perform these operations. The advent of minimally invasive techniques has been associated in retrospective series with lower estimated blood loss (EBL), shorter length of stay (LOS), less postoperative pain, faster recovery and return to work, superior cosmetic results, and lower risk of incisional hernia. Notwithstanding, the robotic approach is associated with increased costs due to a longer operative time and instrument expenditures.
There is a lack of prospective randomized trials comparing R-RPLND to O-RPLND, controlled data is certainly needed. We performed a propensity score matched analysis to limit the impact of selection bias on survival and perioperative outcomes and allow it to approximate results that might be observed in a randomized trial.
Our study used the prospectively maintained eCancerTestis database and we conducted a retrospective chart review of all patients who underwent primary RPLND at the Princess Margaret Cancer Centre between 1990 to 2022. We identified a total of 178 patients who underwent primary RPLND. Of these 137 underwent O-RPLND and 41 R-RPLND. Before PSM, the groups were not balanced, and patients treated with O-RPLND had a larger median retroperitoneal mass size (3.0 vs. 1.7cm), and were less likely to have had elevated tumour markers before pRPLND (22% vs. 7%) We decided to use the following variables for propensity-score matching:
- Age at RPLND
- Obesity (classified as BMI ≥ 30 kg/m2)
- Histology (Seminoma/NSGCT)
- Clinical stage (de novo CSII or CSI and relapsed as CSII)
- Preoperative retroperitoneal mass size (cm)
- Embryonal carcinoma % (orchiectomy pathology)
- Tumor marker status pre-RPLND
- Location of retroperitoneal mass (Paracaval, interaortocaval, paraaortic)
We have described in detail in our article our surgical technique for R-RPLND. The Princess Margaret Cancer Centre philosophy is that while performing R-RPLND we should aim to replicate the open approach at every point in the operation, without sacrificing the oncological safety of the procedure. We perform full bilateral template R-RPLNDs with bilateral nerve sparing when feasible, furthermore, all lumbar arteries and the inferior mesenteric artery (IMA) when not directly involved with disease are preserved. Lastly, all RPLNDs were performed by two expert urologic oncologists each having performed over 500 RPLNDs (MASJ and RJH), and all robotic cases were performed by one surgeon (RJH).
After propensity score matching 26 patients were matched in the R-RPLND (26/41) to 38 in the O-RPLND (38/137) group, and the groups were well balanced.
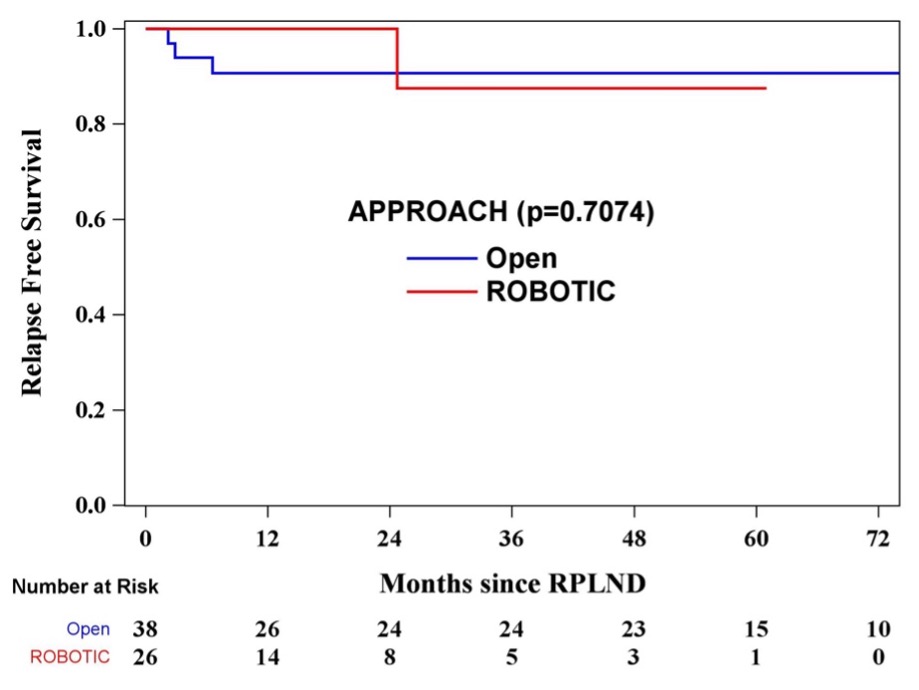
We found no significant differences in RFS between open and R-RPLND at a median follow-up of 23.5 months (HR 0.65, 95% CI 0.07-6.31, p= 0.7097). Of note, among the 4 relapses in the cohort, none were “in field” of the dissection.
R-RPLND was associated with:
- Lower blood loss (median 200 vs. 300cc, p=0.03)
- Reduced length of stay (median 1 vs. 5 days, p<0.0001)
- Longer operative time (median 8.8 vs. 4.3hrs, p<0.0001) *Operative time decreased as experience was gained, but this is also likely offset by an increase in complexity of cases performed robotically as more experience was gained.
- No significant differences in the:
- Complications (p=0.8141) or Grade III complications (p=0.7659)
- Lymph node yield (median 31 vs. 34, p=0.4356)
- RPLND pathology (p=0.6637)
To conclude our study showed that primary robotic RPLND offers low morbidity and improved perioperative outcomes while maintaining the oncological efficacy observed with the open approach and it should be endorsed by clinical practice guidelines provided it is carried out by surgeons at high-volume centres for testis cancer with experience in RPLND.
Written by: Julian Chavarriaga MD, & Robert J. Hamilton MD, MPH, FRCSC
Division of Urology, Department of Surgical Oncology, Princess Margaret Cancer Centre, University Health Network and the University of Toronto, Toronto, Ontario, Canada
Read the Abstract


