We found that testicular cancer survivors had a markedly higher hazard ratio for developing ED and TD compared to non-cancer controls. For ED, we found a hazard ratio of 2.97, while for TD, the hazard ratio was 6.71. We also found high incidence rates of 20.3% and 13.1% at 5 years for ED and TD, respectively in the cancer survivor cohort compared to 5.3% and 1.2%, respectively in the non-cancer controls (Figure 1). Interestingly, while chemotherapy is often implicated in sexual and gonadal dysfunction, our study did not find a significant difference in the incidence of these disorders between patients who received chemotherapy and those who did not (Figure 2).4,5 This finding challenges prevailing narratives that point to chemotherapy as a primary driver of ED and TD and suggests that other factors such as the psychogenic stress associated with a cancer diagnosis and treatment may play a more prominent role.
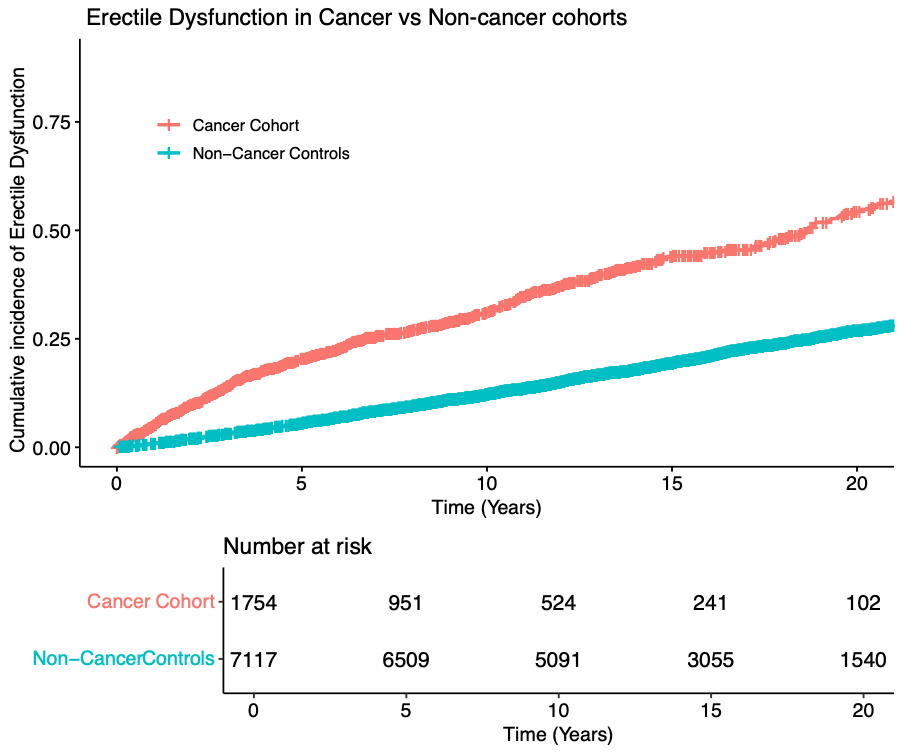
Figure 1: Incidence of Erectile Dysfunction in Cancer vs Non-cancer Cohorts
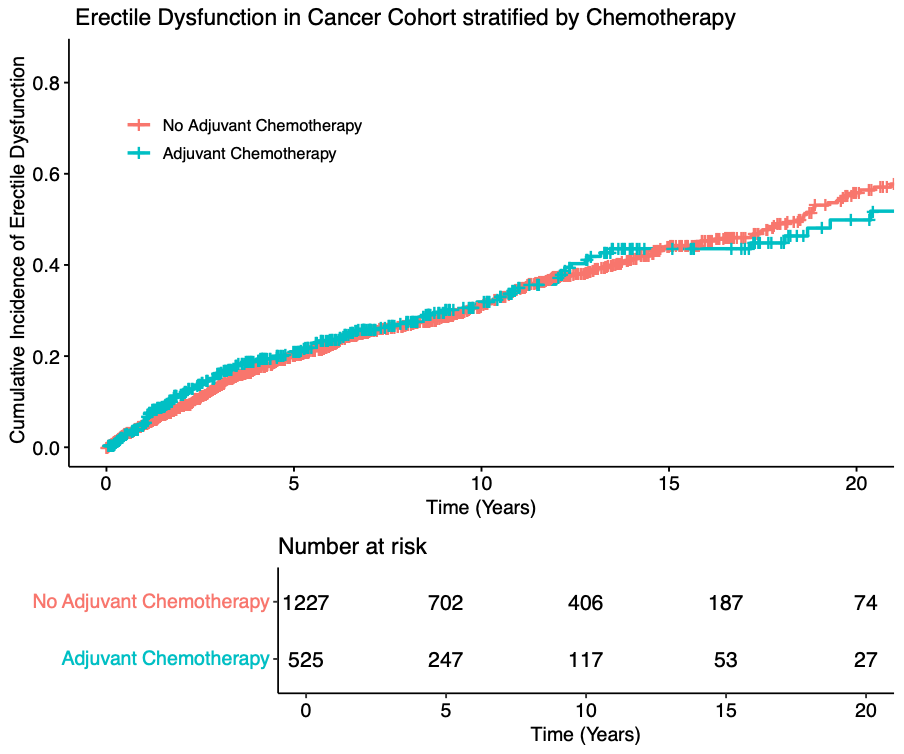
Figure 2: Incidence of Erectile dysfunction in Cancer Cohort when stratified by chemotherapy receipt
The psychogenic component in ED and TD cannot be overlooked. While chemotherapy and other treatments may have direct physiological effects, such as vascular damage or endocrine disruption, the stress of undergoing cancer treatment, grappling with body image changes from orchiectomy, and dealing with the fear of recurrence may further exacerbate these conditions.6,7 Our findings underscore the importance of holistic survivorship care that addresses not only the physiological aftermath of cancer treatment but also the mental and emotional well-being of cancer survivors. As such, it becomes imperative to tailor survivorship care strategies that incorporate mental health support alongside regular sexual health and hormone assessments.
Our study also identified that while ED and TD are more common in TCa survivors, they develop earlier in these patients than in the general population. We support this by reporting median times to the development of ED and TD of 4 and 2.7 years, respectively in TC survivors compared to 9.2 and 8.8 years, respectively in non-cancer controls. This early onset suggests that cancer survivorship exacerbates these processes, pushing these disorders to the forefront much sooner than they would typically emerge.
In conclusion, our study not only highlights the significant risk of ED and TD in testicular cancer survivors but also emphasizes the need for a nuanced approach to survivorship care. By considering the psychogenic and lifestyle factors alongside the direct effects of cancer treatment, we can create more comprehensive and personalized care strategies that improve long-term health outcomes for these patients. Further research should continue to explore these multifactorial etiologies and develop interventions that address both the mind and body in cancer survivorship.
Written by:
- Kshitij Pandit, UC San Diego School of Medicine, San Diego, CA
- Aditya Bagrodia, UC San Diego School of Medicine, San Diego, CA, and UTSW Medical Center, Dallas, Texas
- Pandit K, Riviere P, Morgan K, et al. Incidence of Erectile Dysfunction and Testosterone Deficiency in Testicular Cancer Survivors. J Urol. Published online September 30, 2024. doi:10.1097/JU.0000000000004259
- Rossen P, Pedersen AF, Zachariae R, von der Maase H. Sexuality and body image in long-term survivors of testicular cancer. European Journal of Cancer. 2012;48(4):571-578. doi:10.1016/j.ejca.2011.11.029
- Lackner JE, Märk I, Schatzl G, Marberger M, Kratzik C. Hypogonadism and Androgen Deficiency Symptoms in Testicular Cancer Survivors. Urology. 2007;69(4):754-758. doi:10.1016/j.urology.2007.01.002
- Bandak M, Lauritsen J, Johansen C, et al. Sexual Function in a Nationwide Cohort of 2,260 Survivors of Testicular Cancer after 17 Years of Followup. The Journal of Urology. 2018;200(4):794-800. doi:10.1016/j.juro.2018.04.077
- Sprauten M, Brydøy M, Haugnes H, et al. Longitudinal Serum Testosterone, Luteinizing Hormone, and Follicle-Stimulating Hormone Levels in a Population-Based Sample of Long-Term Testicular Cancer Survivors. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32. doi:10.1200/JCO.2013.51.2715
- Mazzilli F. Erectile Dysfunction: Causes, Diagnosis and Treatment: An Update. Journal of Clinical Medicine. 2022;11(21):6429. doi:10.3390/jcm11216429
- Nargund VH. Effects of psychological stress on male fertility. Nat Rev Urol. 2015;12(7):373-382. doi:10.1038/nrurol.2015.112


