San Francisco, California (UroToday.com) The past few years have ushered several new imaging advances for patients with prostate cancer. While the standard of care in terms of radiologic staging for the vast majority of patients remains the classic CT scan and technetium-99 bone scan, a number of studies have shown improved sensitivity with novel tracers including 18-F choline, prostate-specific membrane antigen (PSMA), 18-F sodium fluoride, fluciclovine F-18, and 11-C acetate, which may be particularly useful in the setting of high risk or recurrent prostate cancer. The most recent diagnostic imaging approval by the FDA was Fluciclovine F18 (Axumin) PET, which was approved in 2016 for men with suspected prostate cancer recurrence based on elevated PSA levels following prior treatment.
The most recent PET probe with both diagnostic and therapeutic potential is 68gallium-labeled PSMA (prostate specific membrane antigen), a transmembrane glycoprotein which was originally cloned out of prostate cancer.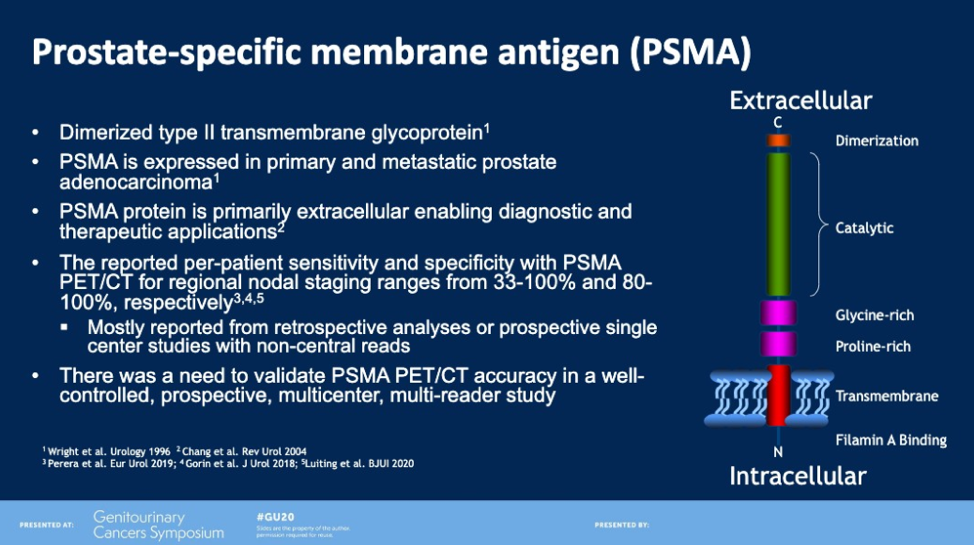
68Ga-PSMA-11 has now been extensively used outside of the United States, and a recent prospective multicenter trial (n=635) done at UCLA and UCSF demonstrated 84% to 92% positive predictive value at 75% overall detection rate in patients with biochemically recurrent prostate cancer and median prostate-specific antigen of 2.1 ng/mL.1 This study demonstrated that even for patients with a PSA <0.5 ng/mL, 38% of patients had PET-positive results, and for patients with a PSA of <5.0, essentially all patients had PET-positive disease (97%). Given the high sensitivity and positive predictive value of PSMA PET, there is significant interest in further developing this radiotracer to enable better detection and treatment of oligometastatic disease.
OSPREY (Observe Prostate Cancer with Accuracy) is a prospective phase II/III multi-center study of 18F-DCFPyL, a targeted small molecular radiopharmaceutical which binds selectively to PSMA with high affinity.
Two cohorts of patients were enrolled – Cohort A included patients with high risk prostate cancer at diagnosis, and Cohort B included recurrent or metastatic prostate cancer. Prior data has been reported at AUA 2019 as well as ASCO 2019 for cohorts A and B. For cohort A, 18F-DCFPyL was 40% sensitive and 98% specific compared with surgical pathology for pelvic lymph nodes, and distant metastatic disease was seen in 11.1% of patients. For cohort B, the sensitivity was 96% overall, with 97% sensitivity in detecting metastatic disease in the bones and lymph nodes, and 100% sensitivity detecting disease in the viscera.2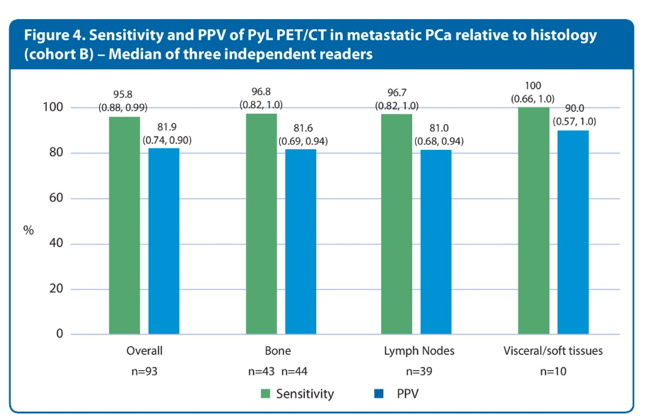
The presentation focuses on the sub-analysis of regional and distant metastases detection rates at initial staging by 18F-DCFPyL PET/CT
Summary
252 men were evaluated in this study. The baseline characteristics are below.
97% of men had no known nodal disease and 99% of men had no known metastatic disease. All men had been planning to undergo radical prostatectomy with lymphadenectomy. 18F-DCFPyL PET/CT revealed nodal disease in 14.7% of patients and metastatic disease in 10.7% of patients. A total of 22% of patients with high risk prostate cancer planned for RP-PLND had regional or distant metastatic lesions detected on 18F-DCFPyL PET/CT.
If you exclude lymph nodes below 5 mm in size which is the limitation of PET detection, the sensitivity of detection increased to 48-62%. One marked example of how 18F-DCFPyL PET/CT changed management is shown below. This was a T1cNxM0 patient by bone scan and on 18F-DCFPyL PET/CT, you can see widespread metastatic disease and thus the patient received systemic therapy rather than surgery.
Conclusions
There is no doubt that PSMA radiotracers are a more sensitive measurement of recurrent and metastatic prostate cancer as compared with traditional imaging techniques. This study, like many others in the PSMA era, demonstrates that metastatic disease may be missed with the typical CT and bone scan, and other studies have shown that this translates into management changes. Another abstract being presented at this ASCO (#292, Impact of 68Ga-PSMA-11 PET on the management of biochemically recurrent prostate cancer in a prospective single-arm clinical trial), demonstrated that intended management change occurred in 260/382 (68%) patients after PSMA imaging. However, it is unknown if earlier detection of oligometastatic disease improves overall survival. Long term follow-up is necessary to determine if these more sensitive techniques are improving overall survival and quality of life, as is mentioned in the limitations of this study.
Presented by: Frederic Pouliot, MD, PhD, Assistant Professor, Department of Surgery, Urology Division, Laval University Hospital Center, Quebec, Canada.
Written by: Jason Zhu, MD. Medical Oncologist, Division of Genitourinary Cancers, Levine Cancer Institute at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California
References:
- Fendler WP, Calais J, Eiber M, et al. Assessment of 68Ga-PSMA-11 PET Accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial. JAMA Oncology 2019;5:856-63.
- Morris MJ, Carroll P, Probst S, et al. A prospective phase 2/3 multicenter study of 18F-DCFPyL PET/CT imaging in patients with prostate cancer: Examination of diagnostic accuracy (OSPREY). American Society of Clinical Oncology; 2018.


