(UroToday.com) The 2023 ESMO annual meeting included a session on prostate cancer, featuring a presentation by Dr. Xiao Wei discussing a post hoc analysis of the VISION trial assessing the prognostic value of neutrophil-to-lymphocyte ratio and lymphopenia in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with 177Lu-PSMA-617. Neutrophil-to-lymphocyte ratio and absolute lymphocyte count is an established prognostic factor in many malignancies. However, the prognostic value of neutrophil-to-lymphocyte ratio and absolute lymphocyte count in patients with mCRPC treated with PSMA-targeted radioligand therapy has not been investigated. At the 2023 ESMO annual meeting, Dr. Wei and colleagues assessed the association of neutrophil-to-lymphocyte ratio and absolute lymphocyte count with 177Lu-PSMA-617 treatment outcomes in patients from the VISION trial.1
Adults with PSMA-positive mCRPC received 177Lu-PSMA-617 (7.4 GBq every 6 weeks, ≤ 6 cycles) + standard of care, or standard of care alone. In this post hoc analysis of VISION, patients were categorized by the following at baseline:
- Neutrophil-to-lymphocyte ratio < 3 vs ≥ 3
- Absolute lymphocyte count < 1.0 × 103/μl vs ≥ 1.0 × 103/μl
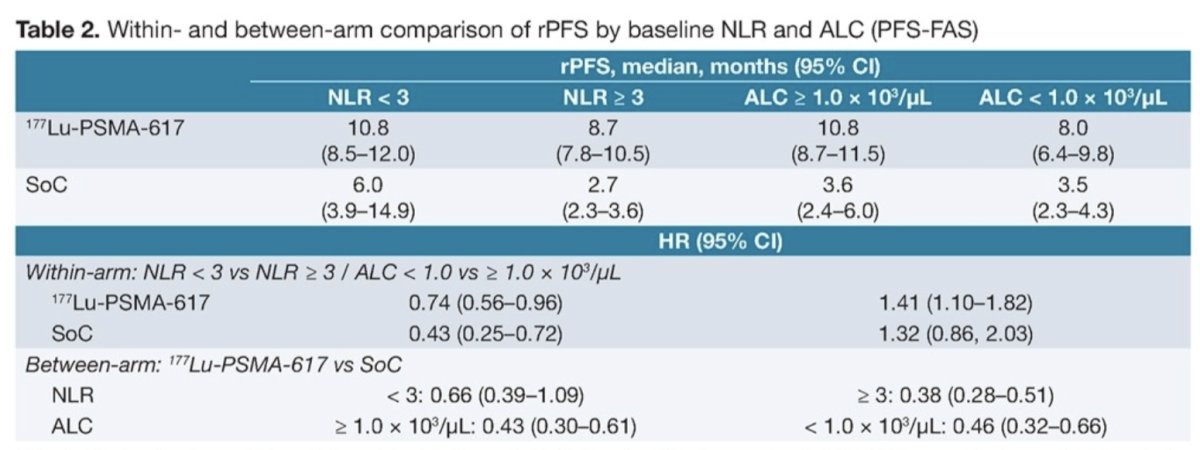
Associations with overall survival (OS) and radiographic progression-free survival (rPFS) were assessed using the Kaplan–Meier method. Hazard ratios were estimated using Cox proportional hazard models.
A total of 714/831 patients (85.9%) in the full analysis dataset had baseline neutrophil-to-lymphocyte ratio and absolute lymphocyte count data available. At baseline, 247/714 patients (34.6%) had a neutrophil-to-lymphocyte ratio <3 and 316/714 (44.3%) had an absolute lymphocyte count <1 x 103/μl. Baseline characteristics were well balanced across subgroups. At baseline, median neutrophil-to-lymphocyte ratio was 3.8 vs 4.0 and median absolute lymphocyte count was 1.06 × 103/μl and 1.0 × 103/μl, for 177Lu-PSMA-617 + standard of care vs standard of care alone, respectively. Median OS and rPFS were prolonged in patients in the 177Lu-PSMA-617 arm compared with the standard of care arm in all subgroups regardless of neutrophil-to-lymphocyte ratio and absolute lymphocyte count:
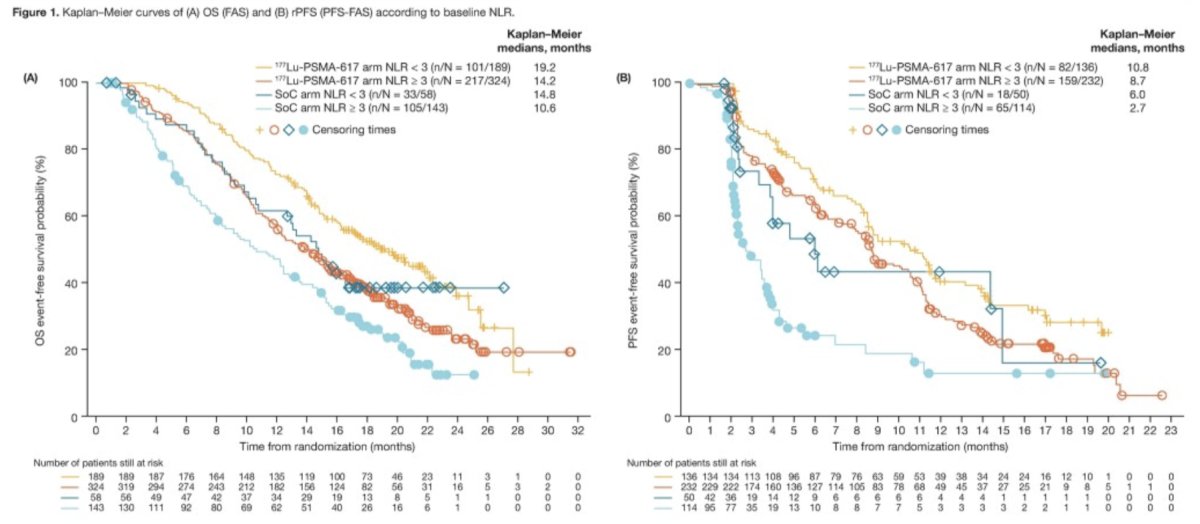
Additionally, median OS and rPFS were longer among patients with baseline neutrophil-to-lymphocyte ratio < 3 than among those with baseline neutrophil-to-lymphocyte ratio≥ 3 in both treatment arms:

Median OS and rPFS were shortest for patients who had consistent baseline and week 6 neutrophil-to-lymphocyte ratio ≥ 3 or absolute lymphocyte count < 1 x 103/μl. Objective response rates were numerically higher among response evaluable patients who had neutrophil-to-lymphocyte ratio ≥ 3 than among those who had neutrophil-to-lymphocyte ratio < 3, and among those who had an absolute lymphocyte count ≥ 1 x 103/μl than those with < 1 x 103/μl. In the 177Lu-PSMA-617 arm, a larger proportion of patients had a PSA response of ≥ 50% and ≥ 80% among those who had a neutrophil-to-lymphocyte ratio ≥ 3 and similarly among those who had an absolute lymphocyte count ≥ 1 x 103/μl than those < 1 x 103/μl. Duration of response was numerically longer among evaluable patients with neutrophil-to-lymphocyte ratio < 3 than those who had ≥ 3, and those with had an absolute lymphocyte count ≥ 1 x 103/μl than those < 1 x 103/μl. Overall, safety results were broadly comparable between subgroups according to baseline neutrophil-to-lymphocyte ratio and absolute lymphocyte count. Generally, these results should be interpreted with caution because the subgroups were not randomized
Dr. Wei concluded her presentation by discussing a post hoc analysis of the VISION trial assessing the prognostic value of neutrophil-to-lymphocyte ratio and lymphopenia in patients with mCRPC treated with 177Lu-PSMA-617with the following concluding statements:
- This post hoc analysis of data from the VISION trial, showed that baseline neutrophil-to-lymphocyte ratio ≥ 3 and absolute lymphocyte count < 1.0 × 103/μl are prognostic for worse OS and rPFS in patients with mCRPC regardless of treatment
- Treatment with 177Lu-PSMA-617 improved OS and rPFS versus standard of care alone regardless of baseline neutrophil-to-lymphocyte ratio or absolute lymphocyte count
- Median rPFS and OS were shortest for patients whose neutrophil-to-lymphocyte ratio remained ≥ 3 or absolute lymphocyte count remained < 1.0 × 103/μl
Presented by: Xiao X. Wei, MD, MAS, Dana-Farber Cancer Institute, Boston, MA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2023 European Society of Medical Oncology (ESMO) Annual Meeting, Madrid, Spain, Fri, Oct 20 – Tues, Oct 24, 2023.
References:
- Sartor O, de Bono J, Chi KN et al. Lutetium-177-PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med. 2021 Sep 16;385(12):1091-1103.


