(UroToday.com) At the WCET 2024 conference, a plenary session focused on the importance of Focal Therapy in robotic practice, with Dr. Indy Gill delivering a compelling presentation. He began by emphasizing his key takeaway: clinical practice should be guided by level 1 evidence, with data-driven planning for localized prostate cancer. Dr. Gill cautioned against treating the entire prostate gland, as it often leads to significant morbidities without offering real oncological benefits. He argued that for men with intermediate-risk prostate cancer, whole-gland treatment might do more harm than good, whereas Focal Therapy presents a balanced approach that can preserve function while maintaining good oncologic outcomes.
Dr. Gill further highlighted a critical gap in the current treatment paradigm for prostate cancer, especially for patients with intermediate risk. He pointed out that the existing binary system—where treatment is either radical or conservative—fails to meet the needs of many patients. This gap has been recognized by patients, physicians, and even the FDA, underscoring the urgent need for less harmful, yet effective, treatments.

Dr. Gill then turned his attention to clinical trials, particularly the ProtecT trial, which he cited as level 1 evidence for prostate cancer treatment. The ProtecT trial followed nearly 1,500 men for 15 years, dividing them into three groups: active monitoring, radical prostatectomy, and radiation therapy.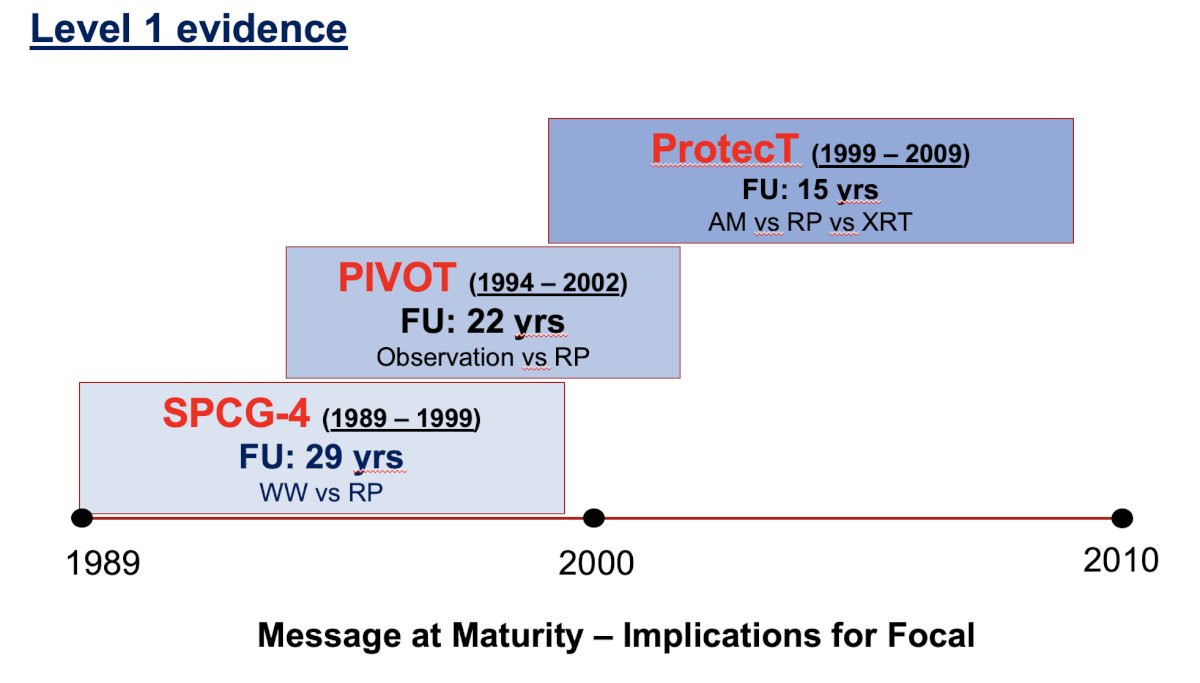
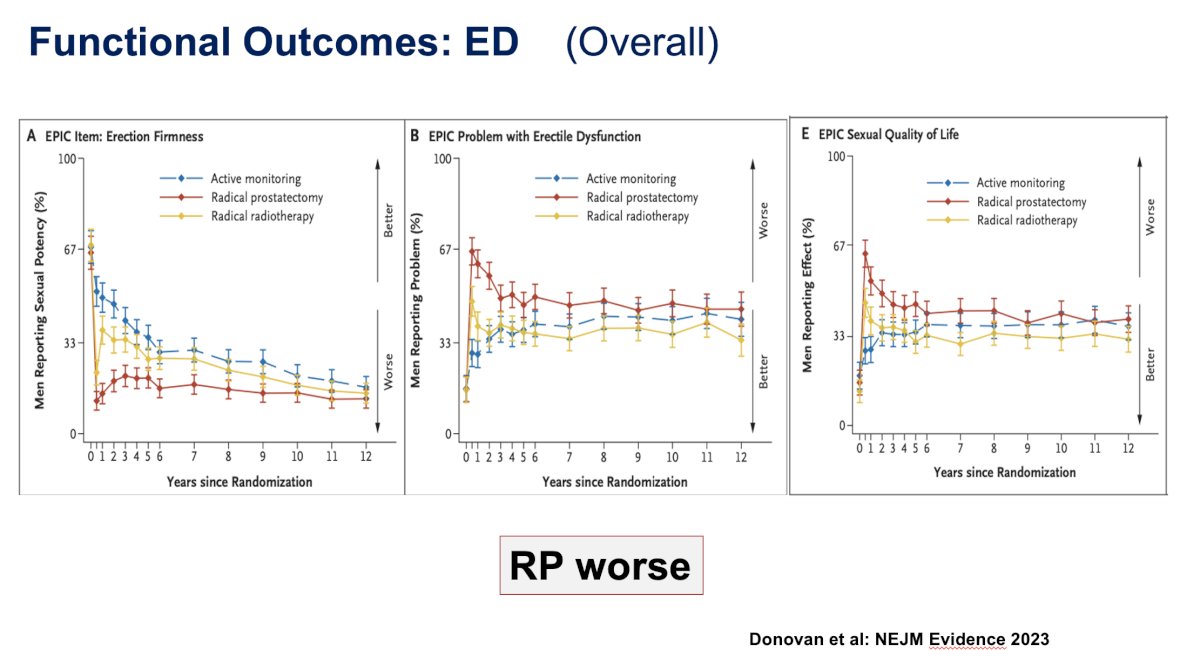
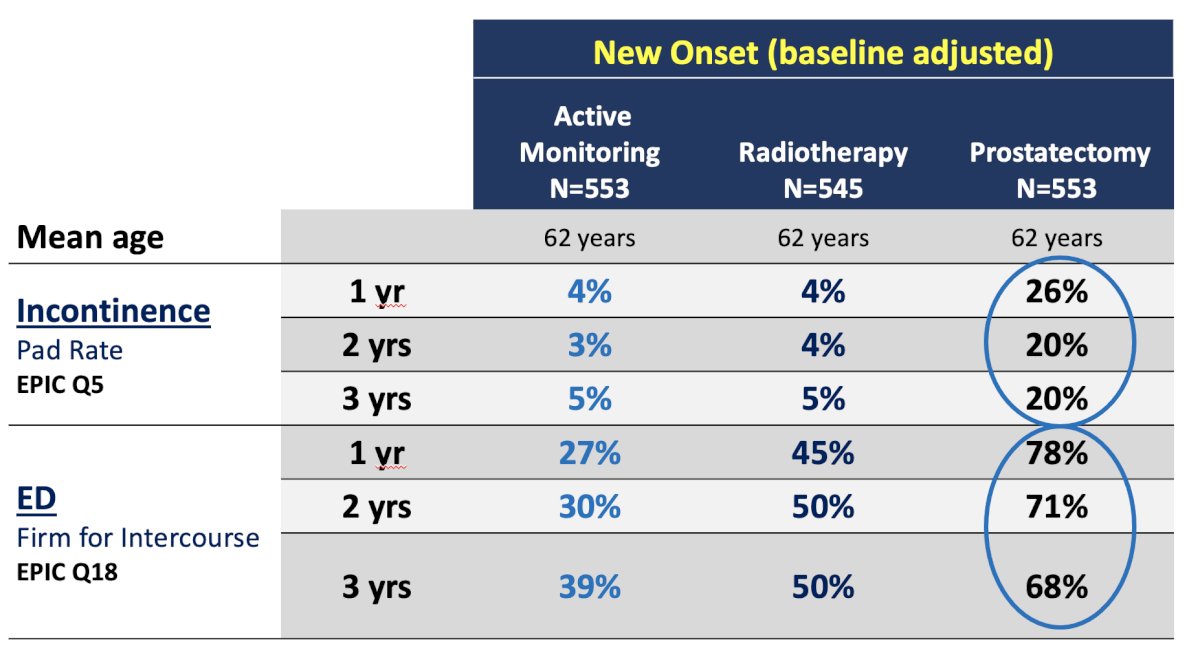
Reviewing the design of the ProtecT trial, Dr. Gill explained that it was conducted across nine U.K. centers between 1999 and 2009, with participants selected based on specific criteria, including being under 70 years old, having a PSA level below 20, and showing no evidence of bone or MRI-detected disease. The primary endpoints were overall survival, cancer-specific survival, distant metastasis, and functional outcomes. Dr. Gill focused first on the functional outcomes, particularly incontinence. He presented data showing that patients who underwent radical prostatectomy experienced worse incontinence compared to those under active surveillance or radiation therapy. Erectile dysfunction was also more prevalent in the radical prostatectomy group. A table illustrated the significantly higher percentages of both incontinence and erectile dysfunction in this group compared to the others, reinforcing the treatment gap Dr. Gill had previously mentioned.

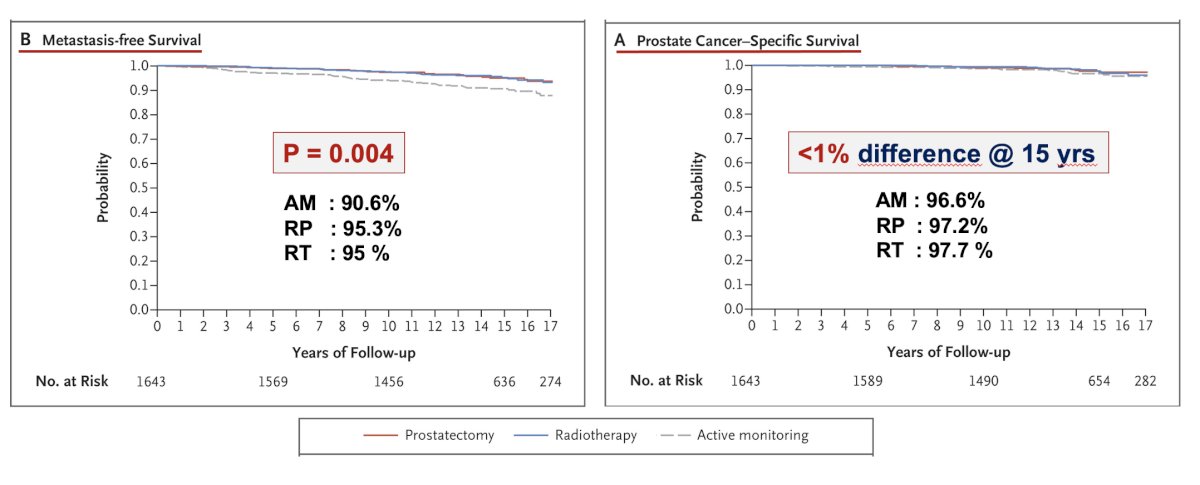
With the ProtecT results pointing to an unmet need for intermediate treatment options, Dr. Gill shifted the discussion to Focal Therapy and radiation therapy. He argued that Focal Therapy strikes a balance by treating the known disease while accepting an acceptable risk of leaving some unknowns untreated. He noted that allowing some GG1 disease to remain might be reasonable, and even a small amount of GG≥2 disease might be manageable under certain circumstances. Dr. Gill emphasized that the ProtecT trial demonstrated that immediate radical therapy for GG≥2 disease might not be necessary, as long as the disease is eventually treated. He further argued that men with intermediate-risk prostate cancer do not need to rush into radical therapy, positioning Focal Therapy as a reasonable bridge between active surveillance and radical treatment.
Dr. Gill also warned that care must be taken with men already diagnosed with GG2 disease, as there is a substantial risk they may harbor occult contralateral GG≥2 disease, which could increase the need for repeat focal therapy. He suggested that Focal Therapy is particularly suitable for low-risk disease in men who demand treatment and for favorable intermediate-risk disease. For low-risk prostate cancer, Focal Therapy offers a good value proposition, as only 1 in 10 patients will have actionable GG≥2 disease after treatment. However, for intermediate-risk prostate cancer, the value is less clear, as 1 in 4 patients may have actionable GG≥2 disease within a few years.
Dr. Gill emphasized the importance of appropriate counseling and setting realistic expectations for patients undergoing Focal Therapy. He introduced the concept of the "Focal Therapy trap," which refers to the risk of out-of-field recurrence requiring additional treatment, leading to more extensive tissue ablation and increased morbidity. Dr. Gill illustrated this with a figure showing the probability of undertreatment relative to gland area and risk. He argued that while ablating more tissue requires more energy and increases morbidity, the ideal treatment would minimize morbidity even as the extent of resection increases. He proposed that efforts should focus on developing non-thermal ablation or resection methods to treat more tissue without increasing morbidity.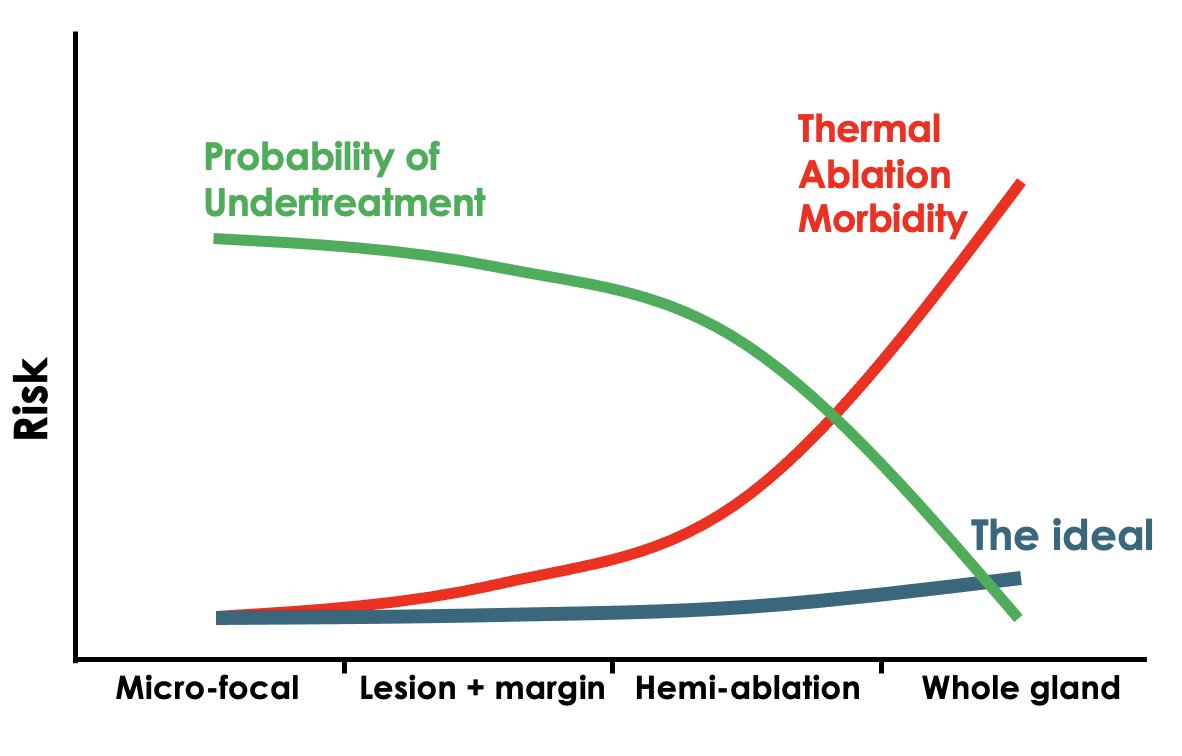
In conclusion, Dr. Gill summarized his key messages: in an ideal world, Focal Therapy could eliminate the need for radical treatments like prostatectomy and radiation therapy. However, even just deferring radical therapy for a few years offers significant benefits. Patients are increasingly interested in Focal Therapy, and it is the responsibility of the medical community to ensure it is done responsibly. In this emerging era of advanced imaging and genomic-based patient-specific risk stratification, treating all patients with robotic prostatectomy is no longer appropriate. He concluded by asserting that while not every practitioner needs to perform Focal Therapy themselves, any program aspiring to be at the cutting edge of urology must have someone on their team who specializes in this important treatment modality.
Presented by: Inderbir Gill MD, University of Southern California, Los Angeles, California.
Written by: Seyedamirvala Saadat, Research Specialist at Department of Urology, University of California Irvine, @Val_Saadat on X during the 2024 World Congress of Endourology and Uro-Technology: August 12 -16, 2024, Seoul, South Korea
References:
- Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, Peters TJ, Turner EL, Martin RM, Oxley J, Robinson M, Staffurth J, Walsh E, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Neal DE; ProtecT Study Group. 10-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Localized Prostate Cancer. N Engl J Med. 2016 Oct 13;375(15):1415-1424.
- Donovan JL, Hamdy FC, Lane JA, Young GJ, Metcalfe C, Walsh EI, Davis M, Steuart-Feilding T, Blazeby JM, Avery KNL, Martin RM, Bollina P, Doble A, Doherty A, Gillatt D, Gnanapragasam V, Hughes O, Kockelbergh R, Kynaston H, Paul A, Paez E, Powell P, Rosario DJ, Rowe E, Mason M, Catto JWF, Peters TJ, Wade J, Turner EL, Williams NJ, Oxley J, Staffurth J, Bryant RJ, Neal DE. Patient-Reported Outcomes 12 Years after Localized Prostate Cancer Treatment. NEJM Evid. 2023 Apr;2(4):EVIDoa2300018.


