Our results about overall survival (OS), progression-free survival ([PFS] time to nodal or metastatic progression), recurrence-free survival (time to local recurrence in the reconstructed penis), and functional outcomes in terms of sexual and lower urinary tract symptoms in patients with squamous cell carcinoma of the penis are thanks to a collaborative prospective database between Hospital Universitario San Ignacio-Pontificia Universidad Javeriana, Universidad Autónoma de Bucaramanga, Hospital Militar Central-Universidad Militar Nueva Granada, and Fundación Santa Fe de Bogotá Universidad de los Andes. All patients are those who underwent organ-sparing surgery (OSS) and immediate reconstruction with a split-thickness skin graft (STSG) since October 2007.
All health institutions involved in the study had a common training on plastic reconstructive OSS of the penis and all the surgeons who collaborated on this multicentric study had the goal that no patient with penile cancer had to undergo mutilating penile surgery without reconstruction again in order to avoid psychological distress, morbidity, and to maintain sexual function. We firmly believe that, if possible, all patients with penile cancer should be treated with OSS and plastic reconstructive surgery of the penis must be offered to them to be carried at the same time as the oncological surgery.
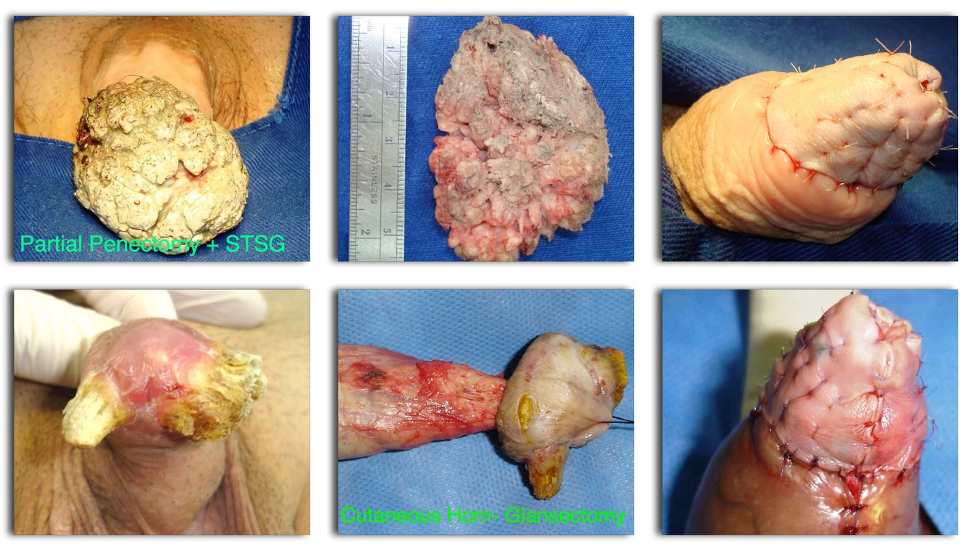
Between October 2007 and September 2019, 57 patients with penile cancer underwent organ-sparing reconstructive surgery with STSG. Twenty were treated with glans resurfacing, 23 with partial splenectomy, and 14 with glansectomy. All cases included intraoperative frozen section pathology and reconstruction was withheld until the pathologist confirmed negative surgical margins intraoperatively. For those who had positive surgical margins, deeper surgical resection was performed until the frozen section was confirmed negative. We did not have a side preference for harvesting the STSG but made sure both thighs were included in the sterile field and avoided skin with hair (see figures).
Interestingly, three patients had nodal disease at the time of surgery documented on a conventional CT scan (one patient on the partial penectomy group and two in the resurfacing group). We used a staged fashion approach in which all patients underwent inguinal lymph node dissection. According to the NCCN penile cancer guidelines, if two or more positive nodes were confirmed after pathologic examination, pelvic lymph node dissection was indicated. Despite the recommendation of the EAU and NCCN penile cancer guidelines for inguinal lymph node dissection (ILND) in patients with intermediate (T1b) and high-risk tumors (≥T2), we didn’t perform pelvic lymph node dissection 13 years ago when we started this series of cases. Unfortunately, one patient (5%) in the resurfacing technique group and seven (30%) in the partial penectomy group initially staged as cN0 who were not initially treated with ILND progressed to nodal disease and curiously these were patients with intermediate-risk not staged with ILND given the reasons aforementioned.
Up to when the follow-up was performed, seven patients had died (12.5%), six due to PC, and 10 (17.8%) had progressed. Kaplan-Meier estimates showed a five-year survival rate of 87.5%, five-year RFS of 98.25%, and a five-year PFS of 83%). Of the seven patients who had died, two had nodal involvement at the time of the diagnosis and despite an adequate lymph node dissection technique they progressed and died of the disease within five years of the initial surgery. Four patients were cN0 at the time of the initial surgery and progressed to nodal involvement, then to metastatic disease, and finally died of PC. The median time for disease progression after surgery in these patients was three (IQR 1.75-12) months.
HRQoL was evaluated with the EuroQol 5D-3L, EQ-VAS that showed a mean global health score of 82.5%. Lower urinary tract symptoms (LUTS) were evaluated with the ICIQ-MLTUS questionnaire. The median voiding score was 4 (IQR 1–15) and the median impact on quality of life was 2 (IQR 0-36). Erectile dysfunction was assessed with the SHIM/IIEF-5 with a median score of 19 (IQR 10.75–25). All of our patients were sexually active (able to have a satisfactory sexual relation, at least monthly) at the time that the questionnaire was answered, except for a patient with advanced Parkinson's disease.
We conclude that organ-sparing reconstructive surgery of the penis remains a safe and viable option for the treatment of localized squamous cell carcinoma (SCC). Reducing morbidity of this mutilating oncological procedure ensuring a favorable appearance of the penis with good HRQoL, preserving urinary and erectile function, without comprising oncological safety. OSS is oncologically equivalent to non-OSS with or without reconstruction and the local recurrence rate is low. Progression to nodal disease is not negligible and all patients with intermediate- and high-risk of nodal involvement must be informed of the risk and offered to stage with ILND after OSS. Immunotherapy ongoing trials (ICONIC) and neoadjuvant and adjuvant chemotherapy roles are currently being evaluated in the International Penile Advanced Cancer Trial (InPACT) and all of these approaches could be helpful to prolong overall survival and PFS in penile cancer patients justifying the need to perform plastic reconstructive OSS.
Based on our results we do not recommend performing this type of surgery if nodal disease is suspected at the time of surgery or if cosmesis or sexual function is not a major concern for the patient and the patient is not seeking to undergo this type of reconstruction.
Take-Home Messages
- Organ-sparing plastic reconstructive surgery (OSS) of the penis remains a safe and viable option for the treatment of localized SCC.
- OSS has shown to reduce morbidity of penile radical surgery, ensuring an aesthetic appearance of the penis, preserving urinary and erectile function, without comprising oncological safety and associated with a good HRQoL.
- OSS showed an estimated five-year survival rate of 87.5% and a five-year PFS of 83%.
- All patients with SCC of the penis, in which an OSS could be considered, should be offered this approach with plastic reconstructive surgery of the penis using an STSG
- Nodal disease remains a critical part of the management of penile cancer, all patients with intermediate- (T1b) and high-risk (≥ T2), cN0 must be considered for ILND which has proven affects PFS and OS.
- Patients with poor prognosis at initial diagnosis cN2,cN3 should be very well selected for OSS, and reconstruction should be withheld or advice against until oncological prognosis has been determined.

Written by: Jaime Pérez, Julián Chavarriaga, Ana Ortiz, Paola Orrego, Sandra Rueda, William Quiroga, Nicolás Fernandez, German Patiño, Verónica Tobar, Nicolás Villareal, Juan Prada, Catalina Barco, Guillermo Sarmiento
Division of Urology, Hospital Universitario San Ignacio. Pontificia Universidad Javeriana. Bogotá, Colombia. Carrera 7 # 40-62; Department of Urology. Fundación Santa Fe de Bogotá. Colombia. Carrera 7 # 117-15. Electronic address: ., Division of Urology, Hospital Universitario San Ignacio. Pontificia Universidad Javeriana. Bogotá, Colombia. Carrera 7 # 40-62. Electronic address: ., Division of Urology. Fundación Oftalmológica de Santander Clínica Ardila Lulle (FOSCAL), Universidad Autonoma de Bucaramanga. Colombia. Av. Gonzalez Valencia # 54-49. Electronic address: ., Division of Urology. Hospital Militar Central, Universidad Militar Nueva Granada. Bogotá, Colombia. Tv. 3C # 49-02. Electronic address: ., Division of Urology. Fundación Oftalmológica de Santander Clínica Ardila Lulle (FOSCAL), Universidad Autonoma de Bucaramanga. Colombia. Av. Gonzalez Valencia # 54-49. Electronic address: ., Division of Urology. Hospital Militar Central, Universidad Militar Nueva Granada. Bogotá, Colombia. Tv. 3C # 49-02. Electronic address: ., Division of Urology, Hospital Universitario San Ignacio. Pontificia Universidad Javeriana. Bogotá, Colombia. Carrera 7 # 40-62; Department of Urology. Fundación Santa Fe de Bogotá. Colombia. Carrera 7 # 117-15; Division of Urology. Hospital for SickKids. University of Toronto. Canada. 555 University Ave, Toronto, ON M5G. Electronic address: ., Division of Urology, Hospital Universitario San Ignacio. Pontificia Universidad Javeriana. Bogotá, Colombia. Carrera 7 # 40-62. Electronic address: ., Division of Urology. Fundación Oftalmológica de Santander Clínica Ardila Lulle (FOSCAL), Universidad Autonoma de Bucaramanga. Colombia. Av. Gonzalez Valencia # 54-49. Electronic address: ., Division of Urology, Hospital Universitario San Ignacio. Pontificia Universidad Javeriana. Bogotá, Colombia. Carrera 7 # 40-62. Electronic address: ., Division of Urology, Hospital Universitario San Ignacio. Pontificia Universidad Javeriana. Bogotá, Colombia. Carrera 7 # 40-62. Electronic address: ., Department of Urology. Fundación Santa Fe de Bogotá. Colombia. Carrera 7 # 117-15. Electronic address: ., Division of Urology. Fundación Oftalmológica de Santander Clínica Ardila Lulle (FOSCAL), Universidad Autonoma de Bucaramanga. Colombia. Av. Gonzalez Valencia # 54-49. Electronic address: .
Read the Abstract


