Since it has been shown that local recurrences occur most often at the location of the macroscopic tumor(s) prior to treatment,9 an alternative strategy to perform dose-escalation is to deliver a simultaneously integrated boost to the intraprostatic tumor(s). This treatment technique was previously demonstrated to be safe and feasible for conventional radiotherapy by the multicentre randomized controlled Phase III Focal Lesion Ablative Microboost in prostatE cancer (FLAME) trial (NCT01168479).10,11
By using hypofractionated whole gland SBRT in conjunction with focal tumor boosting, one could combine the potential advantages of both strategies. This hypothesis was tested in the hypo-FLAME trial delivering 35 Gy in five weekly fractions to the whole prostate gland with an integrated boost up to 50 Gy to the multiparametric MRI-defined tumor (s).12 If the dose constraints to the normal tissue were at risk, these were prioritized over the aimed boost dose.13 No grade ≥ 3 acute GU or GI toxicity was observed. The acute cumulative grade 2 GU and GI toxicity rates were 34.0% and 5.0%, respectively.12
If a significant benefit of focal boosting on (biochemical) disease-free survival would be found by the randomized Phase III FLAME trial, the FLAME schedule may become a new standard of care. Extrapolation of this potential benefit of focal boosting to moderate and extremely hypofractionated treatments should be verified in clinical trials.14 The current Phase II hypo-FLAME trial already showed that a focal SBRT boost to the macroscopic tumor (s) is associated with acceptable acute GU and GI toxicity in addition to whole gland prostate SBRT. Furthermore, besides the potential benefit in tumor control by focal boosting and extreme hypofractionation, the associated reduction in fraction number is attractive to both patients and radiation oncology departments.
Apart from the optimal dose schedule, the impact of shortening the overall treatment time (OTT) in extreme hypofractionated regimens on disease-free survival is currently under investigation as well. King et al. showed there was less rectal toxicity in patients treated every other day compared to consecutive daily treatment.15 Alayed et al. published their results on the impact of the OTT on toxicity, quality of life (QoL), and biochemical failure based in a randomized Phase II study (PATRIOT).16 They compared SBRT (five fractions; 40 Gy) once per week (QW) vs. every other day (EOD) with the OTT varying between 9 and 12 days in the EOD group. Acute urinary and bowel QoL were worse in the EOD group. There was no difference in late toxicity, QoL, or biochemical failure. Further investigation of the optimal OTT of focal boosting SBRT strategies will be performed in the hypo-FLAME 2.0 trial (NCT04045717). An overview of the FLAME consortium trials is shown in Figure 1.
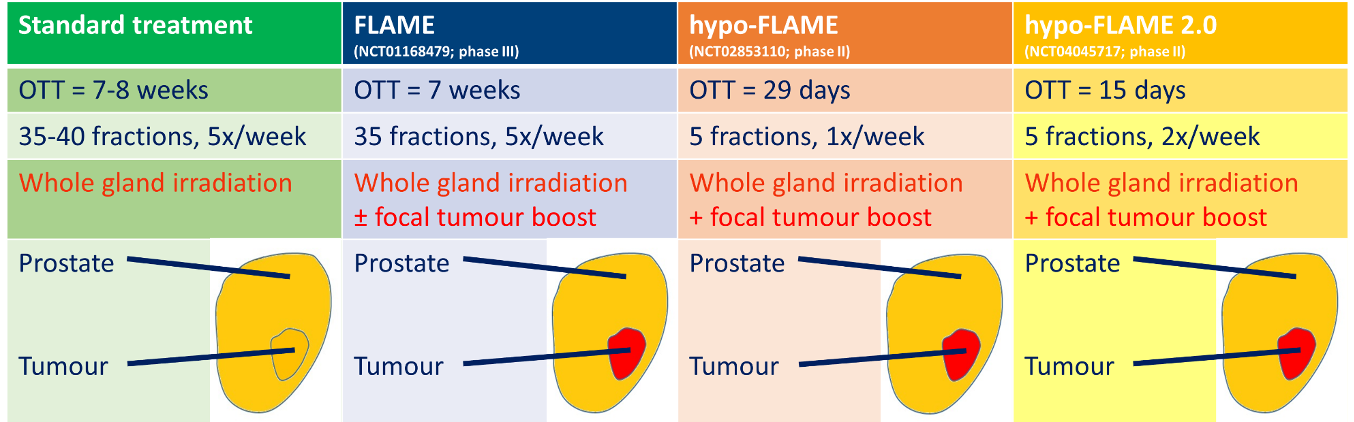
Figure 1. Overview of the FLAME consortium trials investigating focal boosting strategies in prostate cancer
Written by: Cédric Draulans, Department of Radiation Oncology, University Hospitals Leuven, Leuven, Belgium. In collaboration with Floris J. Pos & Uulke A. van der Heide (Department of Radiation Oncology, The Netherlands Cancer Institute, Amsterdam, The Netherlands); Linda G. W. Kerkmeijer, Robert J. Smeenk & Martina Kunze-Busch (Department of Radiation Oncology, Radboud University Medical Centre, Nijmegen, The Netherlands); Veerle H. Groen, Evelyn M. Monninkhof, Hans De Boer & Jochem van der Voort van Zyp (Department of Radiation Oncology, University Medical Centre, Utrecht, The Netherlands); and Sofie Isebaert, Robin De Roover, Tom Depuydt & Karin Haustermans (Department of Radiation Oncology, University Hospitals Leuven, Leuven, Belgium)
References:
- Morgan, Scott C., Karen Hoffman, D. Andrew Loblaw, Mark K. Buyyounouski, Caroline Patton, Daniel Barocas, Soren Bentzen et al. "Hypofractionated radiation therapy for localized prostate cancer: Executive summary of an ASTRO, ASCO, and AUA evidence-based guideline." Practical radiation oncology 8, no. 6 (2018): 354-360.
- Widmark, Anders, Adalsteinn Gunnlaugsson, Lars Beckman, Camilla Thellenberg-Karlsson, Morten Hoyer, Magnus Lagerlund, Jon Kindblom et al. "Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial." The Lancet 394, no. 10196 (2019): 385-395.
- Viani, Gustavo Arruda, Eduardo Jose Stefano, and Sergio Luis Afonso. "Higher-than-conventional radiation doses in localized prostate cancer treatment: a meta-analysis of randomized, controlled trials." International Journal of Radiation Oncology* Biology* Physics 74, no. 5 (2009): 1405-1418.
- Kupelian, Patrick A., Jay Ciezki, Chandana A. Reddy, Eric A. Klein, and Arul Mahadevan. "Effect of increasing radiation doses on local and distant failures in patients with localized prostate cancer." International Journal of Radiation Oncology* Biology* Physics 71, no. 1 (2008): 16-22.
- Zelefsky, Michael J., Xin Pei, Joanne F. Chou, Michael Schechter, Marisa Kollmeier, Brett Cox, Yoshiya Yamada et al. "Dose escalation for prostate cancer radiotherapy: predictors of long-term biochemical tumor control and distant metastases–free survival outcomes." European urology 60, no. 6 (2011): 1133-1139.
- Pahlajani, Niraj, Karen J. Ruth, Mark K. Buyyounouski, David YT Chen, Eric M. Horwitz, Gerald E. Hanks, Robert A. Price, and Alan Pollack. "Radiotherapy doses of 80 Gy and higher are associated with lower mortality in men with Gleason score 8 to 10 prostate cancer." International Journal of Radiation Oncology* Biology* Physics 82, no. 5 (2012): 1949-1956.
- Boike, Thomas P., Yair Lotan, L. Chinsoo Cho, Jeffrey Brindle, Paul DeRose, Xian-Jin Xie, Jingsheng Yan et al. "Phase I dose-escalation study of stereotactic body radiation therapy for low-and intermediate-risk prostate cancer." Journal of Clinical Oncology 29, no. 15 (2011): 2020.
- Kim, DW Nathan, L. Chinsoo Cho, Christopher Straka, Alana Christie, Yair Lotan, David Pistenmaa, Brian D. Kavanagh et al. "Predictors of rectal tolerance observed in a dose-escalated phase 1-2 trial of stereotactic body radiation therapy for prostate cancer." International Journal of Radiation Oncology* Biology* Physics 89, no. 3 (2014): 509-517.
- Cellini, Numa, Alessio G. Morganti, Gian C. Mattiucci, Vincenzo Valentini, Mariavittoria Leone, Stefano Luzi, Riccardo Manfredi, Nicola Dinapoli, and Daniela Smaniotto. "Analysis of intraprostatic failures in patients treated with hormonal therapy and radiotherapy: implications for conformal therapy planning." International Journal of Radiation Oncology* Biology* Physics 53, no. 3 (2002): 595-599.
- Lips, Irene M., Uulke A. van der Heide, Karin Haustermans, Emile NJT van Lin, Floris Pos, Stefan PG Franken, Alexis NTJ Kotte, Carla H. van Gils, and Marco van Vulpen. "Single blind randomized phase III trial to investigate the benefit of a focal lesion ablative microboost in prostate cancer (FLAME-trial): study protocol for a randomized controlled trial." Trials 12, no. 1 (2011): 255.
- Monninkhof, Evelyn M., Juliette WL Van Loon, Marco van Vulpen, Linda GW Kerkmeijer, Floris J. Pos, Karin Haustermans, Laura van den Bergh et al. "Standard whole prostate gland radiotherapy with and without lesion boost in prostate cancer: Toxicity in the FLAME randomized controlled trial." Radiotherapy and Oncology 127, no. 1 (2018): 74-80.
- Draulans, Cédric, Uulke A. van der Heide, Karin Haustermans, Floris J. Pos, Jochem van der Voort van Zyp, Hans De Boer, Veerle H. Groen et al. "Primary endpoint analysis of the multicentre phase II hypo-FLAME trial for intermediate and high risk prostate cancer." Radiotherapy and Oncology 147 (2020): 92-98.
- Draulans, Cédric, Robin De Roover, Uulke A. van der Heide, Karin Haustermans, Floris Pos, Robert Jan Smeenk, Hans De Boer et al. "Stereotactic body radiation therapy with optional focal lesion ablative microboost in prostate cancer: Topical review and multicenter consensus." Radiotherapy and Oncology 140 (2019): 131-142.
- Vogelius, Ivan R., and Søren M. Bentzen. "Diminishing returns from ultra-hypofractionated radiation therapy for prostate cancer." International Journal of Radiation Oncology* Biology* Physics (2020).
- King, Christopher R., James D. Brooks, Harcharan Gill, Todd Pawlicki, Cristian Cotrutz, and Joseph C. Presti Jr. "Stereotactic body radiotherapy for localized prostate cancer: interim results of a prospective phase II clinical trial." International Journal of Radiation Oncology* Biology* Physics 73, no. 4 (2009): 1043-1048.
- Alayed, Yasir, Harvey Quon, Aldrich Ong, Patrick Cheung, William Chu, Hans Chung, Danny Vesprini et al. "Accelerating prostate stereotactic ablative body radiotherapy: Efficacy and toxicity of a randomized phase II study of 11 versus 29 days overall treatment time (PATRIOT)." Radiotherapy and Oncology (2020).


