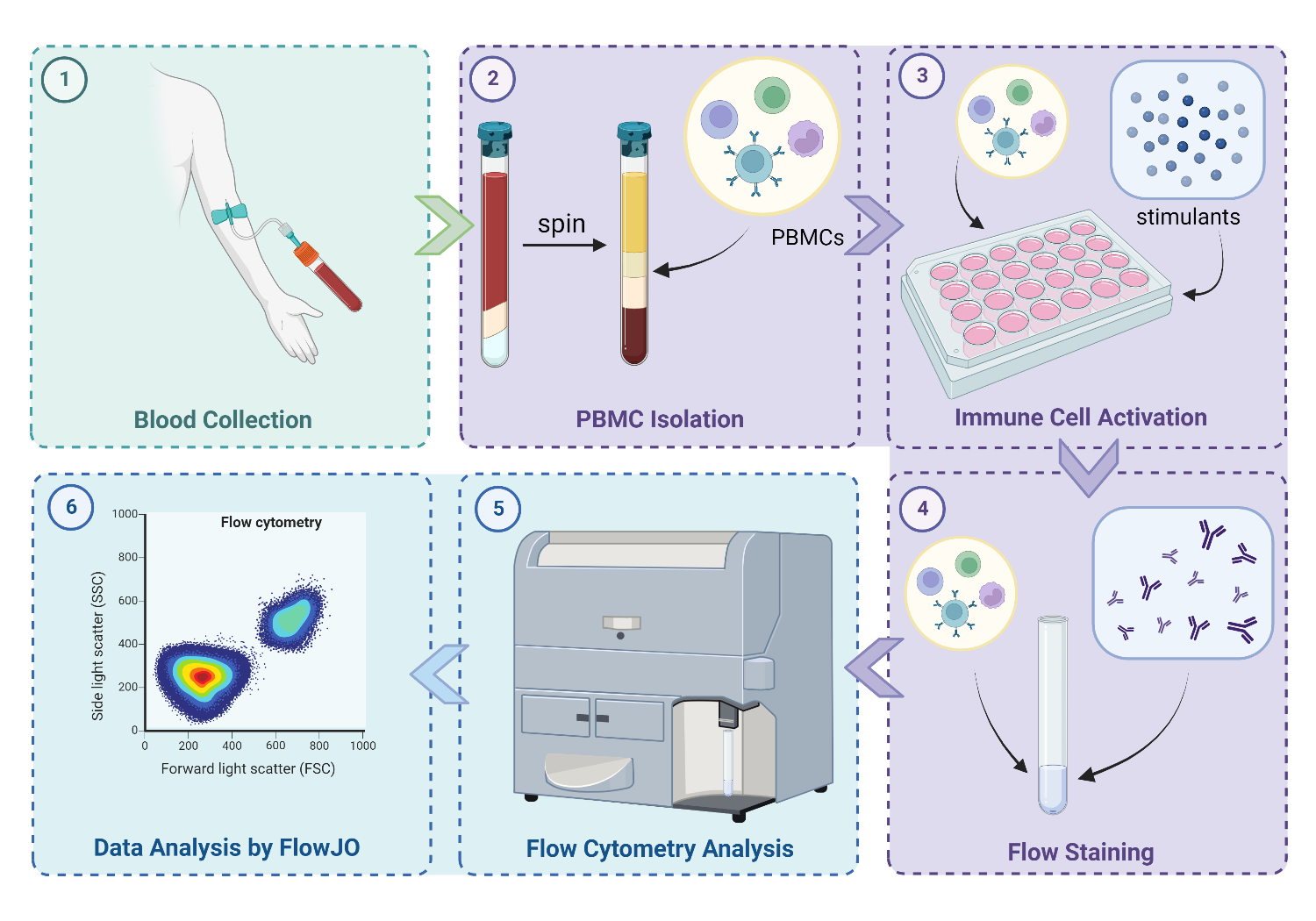
Peripheral blood mononuclear cells (PBMCs) from 16 patients with high-grade Gleason 9 PCa receiving neoadjuvant ADT and radiotherapy (EBRT arm, n = 8; EBRT+BT arm; n = 8) were evaluated for their potential to be leveraged as novel predictive biomarkers.3-5
Overall, a distinct reduction in CD4/CD8 ratio was observed in the EBRT+BT arm, attributed to diminishing CD4+ T helper cells with accumulating surface expression of PD-1 and expansion of CD8+ cytotoxic T cells with increased granzyme B expression. Using re-initiation of systemic therapy as a clinical endpoint, patients with long term response displayed a reduction in CD4+ helper T cells and enrichment of CD8+ cytotoxic T cells, with increased expression of PD-1 and granzyme B respectively. When looking at responsive patients by treatment arm, it is evident the observed changes were attributed to the responsive EBRT+BT cohort.
Our study is the first to directly compare changes in immune cell subsets between EBRT alone and EBRT+BT.6 Together, our results provide evidence that BT, despite being a local treatment, may potentiate T cell activities in the circulation resulting in enhanced systemic control. Expansion of CD8+ T cells with elevated granzyme B activity may suggest a more robust systemic anti-tumour immune response that more effectively eliminates micro-metastasis, leading to improved DMFS seen in patients. With the prevalence of immune checkpoint inhibitors (ICIs), this gives incentive to investigate the use of BT combined with ICIs.7
PBMCs offer several advantages as a biomarker. Evaluating CD4/CD8 ratio in infiltrating lymphocytes from tumour biopsy poses potential complications and repeat biopsy of the prostate is often not readily obtainable and has a small but clinically significant risk of sepsis. PBMCs have the benefit of being non-invasive while having feasibility for serial collection. Furthermore, serum cytokine and granzyme levels may not correlate with trends observed by cellular expression, as they are not necessarily secreted by a single immune population. This highlights the advantage of PBMCs as a predictive biomarker as they allow for the evaluation of distinct proteins and cytokines expressed by specific cell types.
Systemic therapy such as ADT has demonstrated potential to elicit a T cell response.8 Furthermore, patients with favourable response to androgen receptor axis-targeted agents (ARATs) were found to have an elevated T cell population and a proinflammatory cytokine expression compared to patients with poor response.9 Therefore, T cell activation by systemic therapy may be further enhanced when combined with in situ vaccination by radiotherapy for priming of anti-tumour adaptive response.
As the standard of radiotherapy is evolving towards the use of hypofractionation, there is a need to investigate PBMCs as predictive biomarkers for stereotactic body radiation therapy (SBRT), which may modulate circulating immune cell populations and activities.10 Early prediction of radiotherapy response may personalize treatment decisions such as initiation of systemic therapy intensification to further improve patient outcomes.
Written by: Eric Wang,1,2 Danny Vesprini, MD2-4 and Stanley Liu, MD, PhD1-4
- Department of Medical Biophysics, University of Toronto, Toronto, ON
- Sunnybrook Research Institute, Toronto, ON
- Odette Cancer Centre, Sunnybrook Health Sciences Centre, Toronto, ON
- Department of Radiation Oncology, University of Toronto, Toronto, ON
- Kishan AU, Cook RR, Ciezki JP, et al. Radical Prostatectomy, External Beam Radiotherapy, or External Beam Radiotherapy With Brachytherapy Boost and Disease Progression and Mortality in Patients With Gleason Score 9-10 Prostate Cancer. JAMA. Mar 06 2018;319(9):896-905.
- Tang T, Gulstene S, McArthur E, et al. Does brachytherapy boost improve survival outcomes in Gleason Grade Group 5 patients treated with external beam radiotherapy and androgen deprivation therapy? A systematic review and meta-analysis. Clin Transl Radiat Oncol. Jan 2023;38:21-27.
- Eckert F, Schaedle P, Zips D, et al. Impact of curative radiotherapy on the immune status of patients with localized prostate cancer. Oncoimmunology. 2018;7(11):e1496881.
- Du E, Wang L, Li CY, et al. Analysis of immune status after iodine-125 permanent brachytherapy in prostate cancer. Onco Targets Ther. 2017;10:2561-2567.
- Kubo M, Satoh T, Ishiyama H, et al. Enhanced activated T cell subsets in prostate cancer patients receiving iodine-125 low-dose-rate prostate brachytherapy. Oncol Rep. Jan 2018;39(1):417-424.
- Wang H, Mendez L, Morton G, et al. Brachytherapy for high grade prostate cancer induces distinct changes in circulating CD4 and CD8 T cells - Implications for systemic control. Radiother Oncol. Jan 02 2024;191:110077.
- Shiravand Y, Khodadadi F, Kashani SMA, et al. Immune Checkpoint Inhibitors in Cancer Therapy. Curr Oncol. Apr 24 2022;29(5):3044-3060.
- Sutherland JS, Goldberg GL, Hammett MV, et al. Activation of thymic regeneration in mice and humans following androgen blockade. J Immunol. Aug 15, 2005;175(4):2741-53.
- Pal SK, Moreira D, Won H, et al. Reduced T-cell Numbers and Elevated Levels of Immunomodulatory Cytokines in Metastatic Prostate Cancer Patients De Novo Resistant to Abiraterone and/or Enzalutamide Therapy. Int J Mol Sci. Apr 13 2019;20(8)
- Palermo B, Bottero M, Panetta M, et al. Stereotactic Ablative Radiation Therapy in 3 Fractions Induces a Favorable Systemic Immune Cell Profiling in Prostate Cancer Patients. Oncoimmunology. 2023;12(1):2174721.


