EAU 2020
EAU 2020
EAU 2020: The New Testis Cancer Biomarker miRNA 371: Ready for Prime Time?
(UroToday.com) As part of a plenary presentation at the European Association of Urology (EAU) Virtual 2020 meeting assessing “Testis cancer and surgical andrology,” Robert Hamilton, MD, MPH, FRCSC, examined whether miRNA-371 is ready for “prime time” as a testis cancer biomarker.
He began by giving an overview of the landscape of testis cancer in which better biomarkers would aid patient care. These run the gamut from diagnosis and early staging to the provision of chemotherapy and post-chemotherapy retroperitoneal lymph node dissection (RPLND), as well as to reduce the burden of imaging.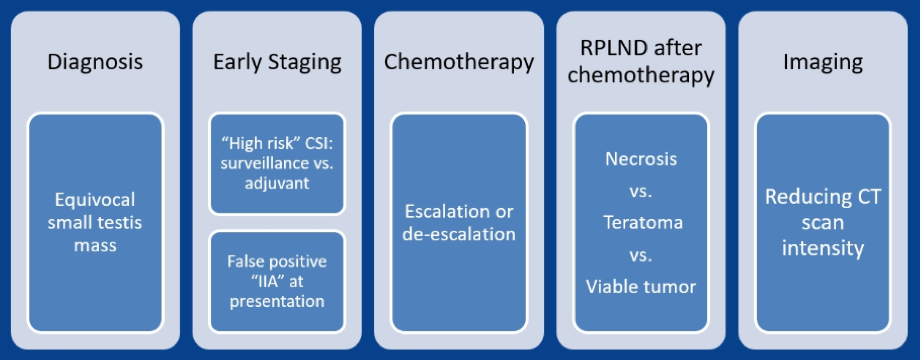
MicroRNA (also called miRNA) are small, single-stranded non-coding RNA fragments. They interact with messenger RNA (mRNA) to influence post-transcription gene expression through translational repression and mRNA degradation. They have been studied as biomarkers in a range of human conditions, including many cancers. This is because miRNA expression is dysregulated in the cancer process with amplification and deletion of miRNA genes; aberrant transcriptional control; epigenetic changes; and altered biogenesis. As suggested by both amplification and deletion leading to carcinogenesis, miRNA may function as either oncogenes or tumor suppressors.
In 2006, Voorhoeve and colleagues were the first to report that miR-371-373 cluster was highly expressed in testis cancer. Subsequent work demonstrated that both the miR-371 cluster and the miR-302 cluster were overexpressed in testis cancer regardless of tumor type (non-seminomatous germ cell tumor (NSGCT) or seminoma), NSGCT subtype, pre- or post-pubertal disease, and anatomic site (gonadal vs. extra-gonadal tumor).
Beyond implication in the relevant biologic processes, miRNA have characteristics which make them well suited as biomarkers: these are detectable in the bloodstream, stable due to their resistance to degradation, and have a short half-life. With a half-life in the range of 3-7 hours, levels fall to 2.6% of pre-orchiectomy levels within 24 hours of surgery. This half-life is much shorter than traditionally utilized biomarkers such as human chorionic gonadotropin (HCG) and alpha-fetoprotein (AFP), which have half-lives of 36 hours and 5-7 days, respectively.
In germ cell tumors (GCTs), two clusters of miRNA are overexpressed:
- The miR-371-373 cluster including: miR-371a-3p, miR-372a-3p, miR-373a-3p
- The miR-302 cluster including: miR-367, miR-302a, miR-302b, miR-302c, miR-302d
Assessing the miR-371 cluster, analysis of miR-371a-3p performed as well in terms of area under the curve (AUC) for the receiver operating characteristic (ROC) curve as a panel of all four miRNA combined (AUC 0.93, 95% confidence interval 0.87 to 0.98).
A recent review article highlighted the main studies of micro-RNAs in germ cell tumors demonstrating very high sensitivity and generally very high levels of specificity as well.
Across the board, the area under the curve (AUC) of the miRNA derived risk prediction models is between 0.87 to 0.97. Thus, we can conclude the miR-371a-3p is very good at detecting when GCT is present, compared to when it was not.
Assessing patients who received chemotherapy and subsequent post-chemotherapy RPLND, Dr. Hamilton discussed a study from his group led by Dr. Ricardo Leao which assessed levels of miR-371a-3p, miR-373-30, and miR-367-3p following orchiectomy but before chemotherapy and following chemotherapy but before RPLND. They compared these levels to clinical characteristics, conventional tumor marks, and PC-RPLND pathology. Expression of miR-371A-3p demonstrated significant differences for patients with viable GCT at PC-RPLND compared to teratoma or fibrosis/necrosis.
The authors then assessed whether serum miR-371a-30 could be useful in guiding treatment decisions. For example, among patients with 1-3cm masses, the authors used the miRNA assay to predict pathology: among 18 patients with a negative miR-371A-3p assay, 8 had teratoma, 10 had necrosis/fibrosis, and none had viable GCT while among 21 with a positive miRNA assay, 6 had viable GCT, 5 had teratoma, and 10 had necrosis/fibrosis. These data suggest that miR-371a-3p can exclude viable disease in patients following chemotherapy. However, teratoma remains a surgical disease so it is less clear whether this can accurately guide treatment.

Dr. Hamilton then highlighted data from Dr. Lafin and colleagues who assessed the association between miR-371a-3p and viable germ cell tumor in patients undergoing RPLND, without prior chemotherapy.
Dr. Hamilton then highlighted ongoing prospective trials including:
- SWOG S182: a prospective observational cohort study to assess miR-371a-3p for outcome prediction in patients with newly diagnosed germ cell tumors. The primary objective of this study is to correlate miR-371 expression with relapse in clinical stage I and IIa disease. Patients will be assessed prior to orchiectomy, post-orchiectomy, and every 3 months for 2 years. The goal is to accrue 1200 patients over 24 months with trial activation occurring very recently, in June 1, 2020.
- AGCT1521: minimizing toxicity for low and standard risk pediatric, adolescent, and young adult germ cell tumor patients. In patients with clinical stage IA/B seminoma or NSGCT, a secondary outcome of this study is to assess the utility of found miRNA, including miR-371-373 and miR-302. Samples are collected prior to orchiectomy and then monthly for 3 months followed by every 3 months for 1 year and every 6 months for another year.
Despite this clinical promise, Dr. Hamilton highlighted limitations of miR-371a-3p including a lack of agreed-upon assay methodology, lack of agreed-upon cut-offs for normal levels, and questions about how to manage patients with teratoma.
Interestingly, tissue-based miRNA assay has found elevated less of miR-375 in teratomas. Thus, if this is validated in serum, the combined use of this with miR-371a-3p may allow for a more comprehensive assessment. However, there are concerns about the reliability of miR-375 to discriminate teratoma.
Presented by: Robert J. Hamilton, MD, MPH, FRCSC, Division of Urology, University of Toronto, Toronto, Canda
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, TN, USA, Twitter: @WallisCJD, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
EAU 2020: Open vs. Minimally Invasive Partial Nephrectomy: What is the Evidence?
(UroToday.com) The European Association of Urology (EAU) Virtual 2020 meeting featured a session on controversies in renal cancer. As part of this session, Maria Carmen Mir Maresma, MD, from Barcelona discussed the evidence for open versus minimally invasive partial nephrectomy. The purpose of partial nephrectomy is to provide negative surgical margins, to maximize renal function preservation, and to perform the procedure with low perioperative morbidity. The adoption of the robotic-assisted approach has increased the number of minimally invasive partial nephrectomies: in 2013 in the United States, 64.1% of partial nephrectomies were performed robotically, 4.8% laparoscopically, and 31.1% open, compared to 2004 when 79.8% of partial nephrectomies were performed open.
Since 2004, Dr. Mir Maresma notes that there have been 1,450 PubMed citations referencing robotic partial nephrectomy. However, many of these studies are (i) by highly skilled surgeons reporting their single-center experience, (ii) for proctoring/intuitive surgery, (iii) published in journals with minimal impact factor, (iv) include no randomized studies, (v) have no few comparative studies, and (vi) no there are adjustments or if there are they are rarely applied.
There are several factors related to partial nephrectomy including pre-surgical, surgical, and post-surgical factors. These are summarized in the following figure:
In a study by Dagenais et al.1 they estimated the relative contributions of patient and surgeon characteristics with regards to key outcomes after partial nephrectomy. Among 1,461 patients, there was significant between-surgeon variability in operative time, estimated blood loss, ischemia time, excisional volume loss, length of stay, positive margins, Clavien complications, and 30-d readmission rate (all p<0.001), but not chronic kidney disease upstaging (p=0.47) or percentage preservation of glomerular filtration rate (p=0.49). Patient factors explained 82% of the variability in excisional volume loss and 0-32% of the variability in the remainder of outcomes. As such, even after adjusting for patient characteristics, there is significant between-surgeon variability in outcomes after partial nephrectomy.
With regards to tumor complexity, several metrics have been reported over the last decade. These include the RENAL score, PADUA score, adhesive perinephric fat Mayo score, and contact surface area. These scoring systems are part of standard reporting of complexity prediction of surgical complications.
There are several resection techniques for patients undergoing partial nephrectomy, including resection (traditional partial nephrectomy), enucleoresection, and simple enucleation. The implications of resection technique are essentially minimal, as surgical margin rates for enucleation (5%) are comparable to enucleoresection (10%), and traditional resection (2%). However, the resection technique and surgical approach are predictors of major complications and acute kidney injury.
The surgical factors impacting partial nephrectomy, stratified by an open versus robotic approach, can be summarized as follows:

Additionally, the host factors impacting partial nephrectomy are as follows:
Dr. Mir Maresma concluded with the following take-home messages from her presentation:
- Oncologic outcomes are similar between open partial nephrectomy and minimally invasive partial nephrectomy
- Renal functional outcomes seem to be slightly better with robotic partial nephrectomy
- There is a large variability of procedures and standardization (resection, surgeon, operative volume, etc)
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, GA, USA, Twitter: @zklaassen_md, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
References:
EAU 2020: Treatment of Recurrent Lymph Node Metastatic Prostate Cancer - Radiation Is the Best Option
EAU 2020: How to Best Approach the Large Renal Mass: Tips and Tricks
EAU 2020: Five Things I Wish I Would Have Known Earlier in My Career: Lessons from the Mentors - Bladder Cancer
Dr. Mark Soloway gave a talk on areas for improvement in bladder cancer, from his significant experience spanning a 50-year time period as a urologist-oncologist, working in many centers across the United States.
EAU 2020: Robotic RPLND is Safe and Feasible
EAU 2020: Controversies in Renal Cancer Surgery: Organ Preservation: Do the Benefits Outweigh Additional Risks? – Pro: Minimally Invasive Nephrectomy
EAU 2020: Open RPLND is Still the Gold Standard
Dr. Nicol began by highlighting the definition of the gold standard which, according to the Collins English Dictionary, as “the supreme example of something against which others are judged or measured.”
EAU 2020: Was Twitter Right? Can We Use SoMe to Better Educate Patients?
(UroToday.com) As part of a plenary presentation at the European Association of Urology (EAU) Virtual Annual Meeting assessing “Testis Cancer and Surgical Andrology”, Juan Luis Vásquez, MD, PhD, highlighted the role of social media, both in urology and more generally.
EAU 2020: How to Manage Testicular Microlithiasis and Carcinoma in Situ
(UroToday.com) As part of a plenary presentation at the European Association of Urology (EAU) Virtual 2020 meeting assessing “Testis cancer and surgical andrology,” Marij Dinkelman-Smit, PhD, outlined an approach to testicular microlithiasis and germ-cell neoplasia in situ (GCNIS).
Dr. Dinkelman-Smit began by highlighting that cure rates for testicular cancer are high following orchiectomy with or without adjuvant therapy as indicated. This paradigm is well established; however, the role of screening of the contralateral testicle with identification of testicular microlithiasis or GCNIS is fraught with significant uncertainty regarding optimal treatment with options including surveillance, orchiectomy, radiotherapy, and chemotherapy. Thus, it leaves open the question of whether we should actively pursue the diagnosis of GCNIS, to offer preventative therapy, with the hopes of improving already high rates of cure.
Dr. Dinkelman-Smit then transitioned to an overview of testicular microlithiasis, which are calcium deposits within the seminiferous tubules, comprising hydroxyapatite core with concentric rings of cellular debris, glycoprotein, and collagen. The etiology is somewhat uncertain but hypothesized mechanisms including inflammation, defective phagocytosis by Sertoli cells, immune response, nanoparticles, or rapid cell turn over. However, she highlighted that testicular microlithiasis are not a precursor lesion for testicular cancer, not are they a causal factor for the development of testicular cancer.
Dr. Dinkelman-Smit highlighted that testicular microlithiasis is a common finding on scrotal ultrasound, present in 2.4-5.6% of asymptomatic men and up to 15% of symptomatic men. Testicular microlithiasis has been associated with testicular cancer, particularly among infertile men in observational cohort. However, there are significant issues with the heterogeneity of the data and shared risk factors.
She recommended a treatment approach driven by reassurance. As with all men, monthly self-examination should be recommended for men with microlithiasis. Ultrasound follow-up, in her estimation, is cost-ineffective. In particularly high-risk patients, biopsy may be considered to exclude GCNIS and cancer.
Transitioning to a discussion of GCNIS, Dr. Dinkelman-Smit highlighted that, unlike testicular microlithiasis, GCNIS may be a precursor lesion to testicular cancer as germ cell tumors are diagnosed in 50% of patients with GCNIS within 5 years and 70% within 7 years. This is an immunohistochemical diagnosis on the basis of testicular biopsy.
GCNIS may be diagnosed adjacent to existing testicular tumors, contralateral to known testicular tumors, and among patients undergoing testicular biopsy for other reasons.
Treatment options for patients with GCNIS include preventative orchiectomy, radiotherapy, surveillance, or chemotherapy. Each of these options has strengths and weaknesses, on the basis of a balance of oncologic control and impairment in testicular function.

In patients who opt for chemotherapy, repeat biopsy to prove resolution of GCNIS is recommended with radiotherapy for those with persistent disease.
Presented by: Marij Dinkelman-Smit, PhD, Erasmus University Medical Center, Rotterdam, The Netherlands
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, TN, USA, Twitter: @WallisCJD, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
EAU 2020: Autologous Testicular Tissue Transplantation in Young Cancer Patients: How Far Are We?
Dr. Orwig began by highlighting the role of fertility preservation in cancer patients. It is well recognized that many cancer treatments can cause permanent infertility. While adult men and women can cryopreserve eggs, sperm, or embryos before treatment for future pregnancies, these options are not available to pre-pubertal patients.
EAU 2020: Infertility and the Risk of Testis Cancer: New Molecular Connections
EAU 2020: Recognising Images, Tissues, Signals
EAU 2020: The Real Effect of Prostate Cancer Treatment: EUPROMS First-Ever Prostate Patient-Driven Quality of Life Study
EAU 2020: Controversies in Renal Cancer Surgery: Do the Benefits Outweigh Additional Risks? — Pro: Partial Nephrectomy
Dr. Breda started by highlighting that several studies have demonstrated the risk of chronic kidney disease associated with metabolic syndrome.
Furthermore, renal cancer surgery also puts patients at risk of chronic kidney disease. Results from the EORTC 30904 randomized trial showed that with a median follow-up of 6.7 years, eGFR <60 was reached by 85.7% with radical nephrectomy as compared to 64.7% for patients undergoing nephron-sparing surgery, with a difference of 21.0% (95% CI, 13.8-28.3).1 Additionally, eGFR <30 was reached by 10.0% for those undergoing radical nephrectomy, compared to 6.3% for those undergoing nephron-sparing surgery, with a difference of 3.7% (95% CI, -1.0 to 8.5). Finally, an eGFR <15 was reached by 1.5% undergoing radical nephrectomy and 1.6% undergoing nephron-sparing surgery, with a difference of -0.1% (95% CI, -2.2 to 2.1).
Dr. Breda notes that the EAU guidelines also support the use of partial nephrectomy when feasible. There is grade 1b evidence that the oncological outcome in terms of overall survival following partial nephrectomy equals that of radical nephrectomy in patients with T1 RCC. There is also a strong recommendation from the guidelines that patients should be offered a partial nephrectomy in the setting of a T1 tumor.
Dr. Breda advocates for a partial nephrectomy even in patients with cT2 tumors if technically feasible, which has been assessed in several studies as summarized below:

Generally, this approach has non-inferior oncological outcomes, lower change in eGFR, possibly better overall survival, but more complications and positive surgical margins.
Recent data from the ROSULA Collaborative Group suggests that a robotic partial nephrectomy for cT2a tumors is both safe and feasible with similar oncologic outcomes [2]. Among 648 patients matched, there were no differences in intraoperative complications (p = 0.478), Clavien-Dindo Grade ≥III complications (p = 0.063), and re-admissions (p = 0.238). Additionally, there was no significant differences for 5-year OS (76.3% vs 88.0%, p = 0.221) and 5-year DFS (78.6% vs 85.3%, p = 0.630) for pT2 RCC, and no differences for 3-year OS (p = 0.351) and 3-year DFS (p = 0.117) for pT3a upstaged RCC. Furthermore, in multivariable analysis, partial vs radical nephrectomy was not associated with all-cause mortality or recurrence.
However, radical nephrectomy was a risk factor for stage III chronic kidney disease (HR 2.51, p<0.001).
Indeed, there is a risk-benefit ratio with regards to complications associated with a difficult partial nephrectomy versus eGFR preservation. A paper published this year from Vilaseca and colleagues3 showed that for tumors with diameters between 7 and 12cm, the risk of eGFR downgrade associated with radical nephrectomy was higher than the risk of complications associated with partial nephrectomy. To summarize this point, the eGFR loss risk in radical nephrectomy is ~40% higher than the complication risk in partial nephrectomy.
Dr. Breda concluded with the following closing remarks:
- The role of partial nephrectomy in cT2 tumors is still debatable but is probably has similar oncological outcomes with better functional outcomes compared to radical nephrectomy
- cT2c partial nephrectomy has worse complication rates and positive margin rates, especially in very complex cases, thus patient selection is key
- cT2 to pT3a upgrading does not seem to affect CSS or OS, thus we should attempt a partial nephrectomy whenever feasible
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
References:
- Scosyrev E, Messing EM, Sylvester R, et al. Renal function after nephron-sparing surgery versus radical nephrectomy: Results from EORTC randomized trial 30904. Eur Urol 2014 Feb;65(2):372-277.
- Bradshaw AW, Autorino R, Simone G, et al. Robotic partial nephrectomy vs minimally invasive radical nephrectomy for clinical T2a renal mass: A propensity score-matched comparison from the ROSULA (Robotic Surgery for Large Renal Mass) Collaborative Group. BJU Int 2020 Jul;126(1):114-123.
- Vilaseca A, Guglielmetti G, Vertosick EA, et al. Value of partial nephrectomy for renal cortical tumors of cT2 or greater stage: A risk-benefit analysis of renal function preservation versus increased postoperative morbidity. Eur Urol Oncol 2020 Jun;3(3):365-371.
Related Content:
EAU 2020: Controversies in Renal Cancer Surgery: Organ Preservation: Do the Benefits Outweigh Additional Risks? – Pro: Minimally Invasive Nephrectomy
EAU 2020: Salvage Lymph Node Dissection in Prostate Cancer: Primary Treatment of Pelvic Lymph Node Metastatic Prostate Cancer - Systemic Only
Dr. van Moorselaar then highlighted the Messing trial assessing immediate versus deferred ADT in patients with node-positive prostate cancer after radical prostatectomy and lymphadenectomy.3 This trial had 98 patients randomized to receive immediate ADT (n=47) or to be observed (n=51), with ADT to be given on detection of distant metastases or symptomatic recurrences. At median follow-up of 11.9 years (range 9.7-14.5), men assigned immediate ADT had a significant improvement in overall survival (HR 1.84, 95% CI 1.01-3.35), prostate-cancer-specific survival (HR 4.09, 95% CI 1.76-9.49), and progression-free survival (HR 3.42, 95% CI 1.96-5.98). Dr. van Moorselaar notes that issues for this trial were that there was no central pathology review and that there were 220 patients planned, but only 98 in the trial. Furthermore, there was lower cancer-specific survival in the observation group compared to two other series (78% after 5 years versus 91%). Additionally, there was no baseline prostate-specific antigen (PSA) testing and recruitment was at 36 institutions, potentially leading to heterogeneity in management.
Dr. van Moorselaar also highlighted the EORTC 30846 trial which evaluated the effect of early versus delayed hormone treatment in pN1-3 prostate cancer.4 There were 254 men randomized and in the ITT analysis, there was a 22% increase in the hazard of death of those randomized to delayed treatment (HR 1.22, 95% CI 0.92, 1.62). Additionally, the median overall survival (OS) in the immediate treatment group was 7.6 years (95% CI, 6.3-8.3 years) versus 6.1 years (95% CI, 5.7-7.3 years) in the delayed treatment group.
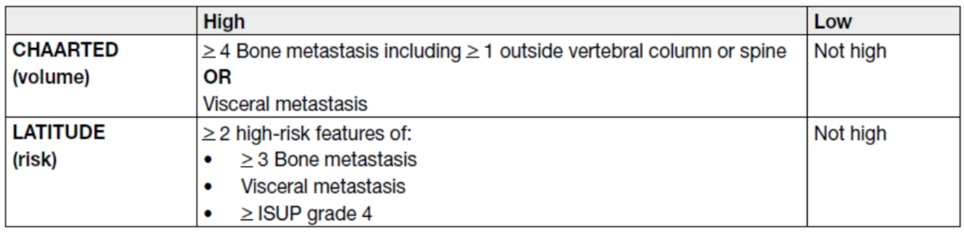
Data from the CHAARTED trial has recently been extracted to outcomes by volume of disease.5 For patients with the high-volume disease (n = 513), the median OS was 51.2 months with chemohormonal therapy versus 34.4 months with ADT alone (HR 0.63, 95% CI 0.50-0.79). For patients with low-volume disease (n = 277), there was no OS benefit was observed (HR 1.04, 95% CI 0.70-1.55):

In the ARCHES trial, patients with predominately high-volume disease were randomized to enzalutamide + ADT or ADT alone. Notably, 17% of the cohort had previously received docetaxel. While OS data from this cohort is immature, the addition of enzalutamide was found to reduce the risk of radiographic progression versus ADT plus placebo by 61% (HR 0.39, 95% CI 0.30-0.50) [6]. The ENZAMET trial also utilized enzalutamide but had ~50% of patients with high-volume disease. Interim analysis after a median follow up of 34 months from this trial showed a significant survival benefit in the enzalutamide group versus those receiving standard nonsteroidal anti-androgens (HR 0.67 95% CI 0.52-0.86) [7].
Dr. van Moorselaar concluded highlighting the EAU guidelines that there is strong evidence to suggest that men should be offered ADT in combination with docetaxel for men that present with M1 disease who are fit for chemotherapy. Additionally, men may also consider the option of abiraterone or apalutamide or enzalutamide for those that are fit for these regimens.
Presented by: Jeroen van Moorselaar, MD, PhD, VU University Medical Centre, Amsterdam, The Netherlands
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, GA, USA, Twitter: @zklaassen_md, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
References:
- Sweeney CJ, Chen YH, Carducci M, et al. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med. 2015;373(8):737-746.
- Fizazi K, Tran N, Fein L, et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N Engl J Med. 2017;377(4):352-360.
- Messing EM, Manola J, Yao J, et al. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol 2006 Jun;7(6):472-479.
- Schroder FH, Kurth KH, Fossa SD, et al. Early versus delayed endocrine treatment of T2-T3 pN1-N3 M0 prostate cancer without local treatment of the primary tumour: Final results of European Organization for the Research and Treatment of Cancer protocol 30846 after 13 years of follow-up (a randomized controlled trial). Eur Urol 2009 Jan;55(1):14-22.
- Kyriakopoulos CE, Chen YH, Carducci MA, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer: Long-term survival analysis of the randomized phase III E3805 CHAARTED trial. J Clin Oncol 2018 Apr 10;36(11):1080-1087.
- Armstrong AJ, Szmulewitz RZ, Petrylak DP, et al. ARCHES: A Randomized, Phase III Study of Androgen Deprivation Therapy with Enzalutamide or Placebo in Men with Metastatic Hormone-Sensitive Prostate Cancer. J Clin Oncol. 2019 Nov 10;37(32):2974-2986.
- Davis ID, Martin AJ, Stockler MR, et al. Enzalutamide with Standard First-Line Therapy in Metastatic Prostate Cancer. N Engl J Med 2019 Jul 11;381(2):121-131.
EAU 2020: What Are the Consequences for Implants in Urology with the New EU Directive?
EAU 2020: Five Things I Wish I Would Have Known Earlier in My Career: Lessons from the Mentors - Prostate Cancer
(UroToday.com) Dr. Peter Carrol began his talk stating one general thing that can still improve, and this was the reduction of disparities in care affected by ethnicity, gender, insurance and education, geographic distance, and disparities specific to the LGBTQ community. Urology can help in this matter by allowing itself to be a more diverse and welcoming specialty.


