Introduction
In 2021 in the United States, there will be approximately 83,730 new cases of bladder cancer (~64,280 men and 19,450 women) and approximately 17,200 deaths from bladder cancer (12,260 men and 4,940 women). On a global scale, in 2017 it was estimated that there were 2.63 million (95% CI 2.57-2.72 million) bladder cancer cases, involving 2.03 million (95% CI 1.96-2.11 million) men and 0.60 million (95% CI 0.58-0.62 million) women.1 As such, although bladder cancer may be a lethal diagnosis for some, there are also millions of bladder cancer survivors worldwide. Bladder cancer patients, generally, have a higher level of comorbidity than most other patients with genitourinary malignancies, and recent literature over the last 5 years or so suggests that bladder cancer patients have proportionately worse depression and mental health, as well as being at increased risk of suicidal death when compared to the general population. This article will discuss the impact of depression and mental health associated with a bladder cancer diagnosis, assess the impact of a bladder cancer diagnosis on risk of suicide, and discuss future endeavors and areas of focus for improving outcomes for patients with bladder cancer.
Depression and Anxiety
In Western countries, the lifetime prevalence of major depression is estimated at 16.5%. Work from >30 years ago from the Psychological Collaborative Oncology Group suggested that 47% of adult patients with cancer were maladjusted to an illness crisis, with the most common manifestation being adjustment disorder with depression. In 2018, Vartolomei and colleagues2 performed a systematic review of the literature assessing the prevalence of depression and anxiety among patients with bladder cancer, including 13 studies encompassing 1,659 patients. Six studies assessed depression prior and after treatment at 1, 6, and 12 months, whereas four studies investigated anxiety, and seven additional studies reported the prevalence of depression and anxiety among patients with bladder cancer at a specific time-point. Overall, pretreatment depression rates ranged from 5.7 to 23.1% and post-treatment from 4.7 to 78%, while post-treatment anxiety rates ranged from 12.5 to 71.3%.
Compared to the prostate cancer literature, there is a relative paucity of data assessing how specific aspects of treatment may affect depression scores amongst bladder cancer patients. In a single-center setting, Zhang et al.3 evaluated anxiety, depression, and quality of life by patients' self-reported scales, as well as predictive factors for anxiety and depression exacerbation among 194 muscle-invasive bladder cancer patients receiving adjuvant chemotherapy after radical cystectomy. The Hospital Anxiety and Depression Scale (HADS) was used to evaluate anxiety and depression, and the EORTC QLQ-C30 Scale was used to assess quality of life. After adjuvant chemotherapy, this study found that HADS-Anxiety score (p = 0.042), anxiety percentage (p = 0.036), HADS-Depression score (p < 0.001), depression percentage (p = 0.002) and the EORTC QLQ-C30 Functional score (p = 0.002) were increased compared with baseline. Furthermore, on multivariable analysis, increasing age (p < 0.001), increasing BMI (P = 0.021) and hypertension (P = 0.001) were associated with worsening of the HADS-Anxiety score, while male gender (P < 0.001) was associated with worsening of HADS-Depression score during adjuvant chemotherapy.
Taken together, given the prevalence of bladder cancer and the associated post-diagnosis/treatment depression and anxiety that occurs, this is an actionable patient population for targeting psycho-oncology intervention, particularly in the comorbid, elderly, and male patients that are particularly at risk of depression or anxiety.
Broader Mental Health Considerations
Although the majority of bladder cancer literature has been dedicated to optimizing oncological outcomes and focuses on physical prognostic criteria, emerging data have suggested that both pre-and post-treatment mental health (not just isolated to depression) may play as important a role in patient outcomes as physical health. In a systematic review assessing the prevalence and impact of mental health disorders in bladder cancer patients, Pham et al.4 identified 87 publications that met initial inclusion criteria, leading to 19 relevant publications incorporated into the review, of which 11 were prospective studies and 8 were retrospective studies. They found that mental health issues, such as depression and anxiety, often coexist with a diagnosis of bladder cancer. Further, those with a worse oncologic prognosis have a greater psychological burden. Additionally, poor mental health was associated with adverse treatment outcomes such as postsurgical complication rates and survival outcomes.
A similar study to characterize the patterns of care and survival of elderly patients with a pre-existing mental illness diagnosed with bladder cancer was undertaken by Sathianathen et al.5 using the SEER-Medicare database. This study included elderly patients (≥68 years old) with localized bladder cancer from 2004 to 2011, stratified by the presence of a pre-existing mental illness at the time of cancer diagnosis: severe mental illness (consisting of bipolar disorder, schizophrenia, and other psychotic disorders), anxiety, and/or depression. The authors examined
the stage at presentation and receipt of guideline-concordant therapies (ie. radical cystectomy for muscle-invasive disease). Among 66,476 patients meeting inclusion criteria, 6.7% (n = 4,468) had a pre-existing mental health disorder at the time of cancer diagnosis. These patients were significantly more likely to present with muscle-invasive disease than those with no psychiatric history (23.0% vs 19.4%, p < 0.01). In patients with muscle-invasive disease, those with severe mental illness (OR 0.55, 95% CI 0.37-0.81) and depression only (OR 0.71, 95% CI 0.58-0.88) were significantly less likely to undergo radical cystectomy or trimodality therapy. However, patients in this subgroup who underwent radical cystectomy had significantly superior overall (HR 0.54, 95% CI 0.43-0.67) and disease-specific survival (HR 0.76, 95% CI 0.58-0.99) compared with those who did not receive curative treatment.
Pre-cancer diagnosis utilization of psychiatric resources has been suggested as a more accurate assessment of mental health comorbidity burden at the population level rather than relying on specific ICD-9/ICD-10 codes for mental health illnesses. To assess this impact in a Canadian health care setting, Klaassen et al.6 included all residents of Ontario diagnosed with one of the ten most prevalent malignancies (which included bladder cancer) from 1997 to 2014. A psychiatric utilization grade (PUG) score in the five years prior to a cancer diagnosis was calculated as follows: 0 – none; 1 – outpatient psychiatric utilization; 2 - emergency department psychiatric utilization; and 3 – psychiatric specific hospital admission. A total of 676,125 patients were included, specifically 359,465 (53.2%) with PUG score 0, 304,559 (45.0%) with PUG score 1, 7,901 (1.2%) with PUG score 2, and 4,200 (0.6%) with PUG score 3. Increasing PUG score was independently associated with worse cancer-specific morality, with an effect gradient across the intensity of pre-diagnosis psychiatric utilization (vs PUG score 0): PUG score 1 HR 1.05 (95% CI 1.04-1.06), PUG score 2 HR 1.36 (95% CI 1.30-1.42), and PUG score 3 HR 1.73 (95% CI 1.63-1.84). In a subgroup analysis specific to anatomic site, bladder cancer patients with pre-diagnosis psychiatric utilization of resources worse cancer-specific morality with increasing PUG score (vs PUG score 0): PUG score 1 HR 1.09 (95% CI 1.03-1.14), PUG score 2 HR 1.29 (95% CI 1.02-1.64), and PUG score 3 HR 2.18 (95% CI 1.62-2.93).
Several studies among bladder cancer patients have also assessed the impact of post-diagnosis mental health diagnosis on outcomes and survival. Using the SEER-Medicare database from 2002 to 2011, Jazzar and colleagues7 identified 3,709 patients who were diagnosed with clinical stage T2 through T4a bladder cancer of which 1,870 (50.4%) were diagnosed with posttreatment psychiatric disorders. Patients who underwent radical cystectomy were identified as being at significantly greater risk of having a posttreatment psychiatric illness compared with those who received radiotherapy and/or chemotherapy (HR 1.19, 95% CI 1.07-1.31):

Furthermore, in adjusted analyses, diagnosis of a psychiatric disorder resulted in significantly worse overall survival (HR 2.80, 95% CI, 2.47-3.17) and cancer-specific survival (HR 2.39, 95% CI, 2.05-2.78).
This same group of investigators also used the SEER-Medicare database to assess prescription patterns and predictors in older patients with bladder cancer.8 This cohort comprised 10,516 patients diagnosed with clinical stage T1-T4a, N0, M0 bladder urothelial carcinoma from 2008 to 2012 of which 5,621 (53%) were prescribed psychotropic drugs following bladder cancer diagnosis. Overall, 3,972 (38%) patients had previous psychotropic prescriptions prior to cancer diagnosis, and these patients were much more likely to receive a post-cancer diagnosis prescription. Additionally, prescription rates for psychotropic medications were higher among patients with higher stage bladder cancer (p < 0.001). Gamma-aminobutyric acid modulators/stimulators and serotonin reuptake inhibitors/stimulators were the highest prescribed psychotropic drugs in 21% of all patients. Furthermore, adherence for all drugs was 32% at three months and continued to decrease over time.
Recent work from Ontario has also delineated the rate of post-curative intent cystectomy/radiotherapy utilization of mental health services. Using the Ontario Cancer Registry (2004-2013) to identify 4,296 patients that underwent radical cystectomy (n = 3,332) or curative radiotherapy (n = 964), Raphael et al.9 assessed mental health service use (defined as a visit to a general practitioner, psychiatrist, emergency department or hospitalization), specifically assessing baseline, peri-treatment, and post-treatment mental health service use. Compared to baseline, the rate of mental health service use was higher in the peri-treatment (aRR 1.64, 95% CI 1.48-1.82) and post-treatment periods (aRR 1.45, 95%CI 1.30-1.63), and by 2-years post-treatment, 24.6% (95% CI 23.4%-25.9%) of all patients had utilized mental health services:
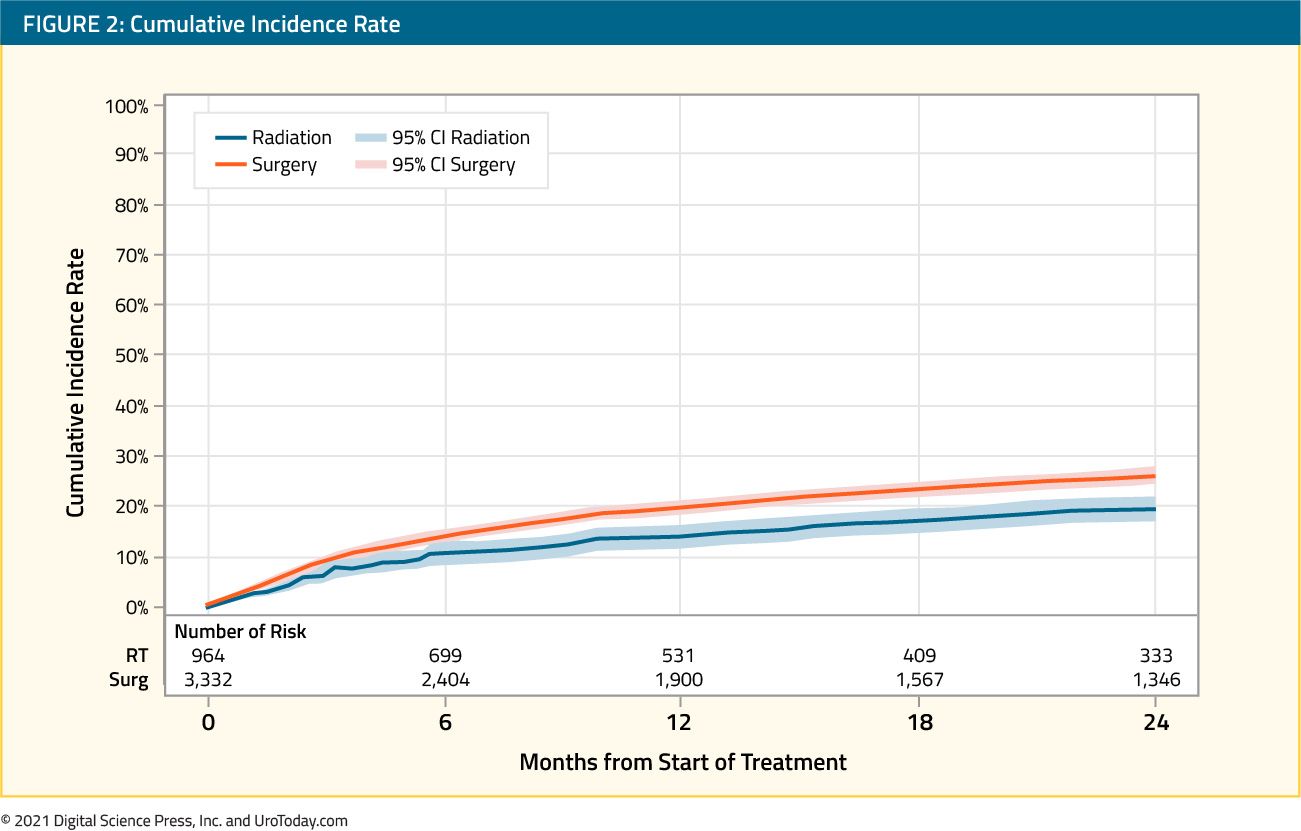
Patients with baseline mental health service use had substantially higher mental health service use in the peri-treatment (aRR 5.77, 95% CI 4.86-6.86) and post-treatment periods (aRR 4.58, 95% CI 3.78-5.55). Additionally, female patients had higher use of mental health services overall, but males had a higher incremental increase in the post-treatment period compared to baseline.
Over the last several years, population-level studies have assessed the impact of pre-and post-bladder diagnosis mental health illness. Elderly patients with muscle-invasive bladder cancer and a pre-existing mental disorder are less likely to receive guideline-concordant management, which leads to poor overall and disease-specific survival. Furthermore,
half of bladder cancer patients with muscle-invasive bladder cancer who undergo treatment are subsequently diagnosed with a psychiatric disorder, resulting in worse survival outcomes compared with patients who do not have a posttreatment psychiatric diagnosis. Over half of these patients receive a psychotropic prescription within two years of their cancer diagnosis, however there appears to be low adherence to medication use, which emphasizes prolonged patient monitoring and further investigation.
Suicide
Globally, nearly 800,000 people die of suicide every year, accounting for 1.4% of deaths worldwide. Over the last decade, there have been several studies noting that suicide rates among cancer patients appear to be higher than the general population,10 including patients with genitourinary malignancies.11 Among cancer patients, patients with bladder cancer have one of the highest suicide rates. In the SEER database, over a 40-year time frame (1973-2013), 794 patients with bladder cancer (0.24%) died of suicide, 190,734 patients (57.2%) died from other causes, and 142,151 patients (42.6%) were alive.12 Significant factors associated with suicide included being unmarried (vs married: HR 1.74, 95% CI 1.49-2.04), white race (vs black: HR 2.22, 95% CI 1.32-3.74), male (vs female: HR 6.91, 95% CI 5.04-9.47), have regional disease (vs. localized: HR 2.49: 2.05-3.03), live in the Southeast United States (vs. Northeast: HR 2.43, 95% CI 1.78-3.32), not undergo a radical cystectomy (vs cystectomy: HR 1.42, 95% CI 1.03-1.94), and increasing age (>= 80 years vs 60-69 years: HR 1.32, 95% CI 1.06-1.66). As follows are suicide rates per 100,000 person-years of follow-up by a decade of bladder cancer diagnosis:

Guo et al.13 recently published a systematic review to assess how bladder cancer increases suicide risk and to identify demographic and clinical factors associated with suicidal death. This review identified five retrospective cohorts comprising 563,680 patients with bladder cancer. Higher risk of suicide by 1.90-fold was observed among patients with bladder cancer (HR 1.90, 95% CI 1.29-2.81, p = 0.001, I2 = 81.2%), especially in patients older than 70 years of age (HR 1.36, 95% CI 1.29-1.43, p < 0.00, I2 = 0%), those that are unmarried (HR 1.72, 95% CI 1.61-1.83, p < 0.001, I2 = 0%), and those with regional bladder cancer (HR = 1.88, 95% CI: 1.10-3.21; P = 0.021; I2 = 96.3%), compared to those without bladder cancer. In this systematic review, gender and race were not associated with increased suicide risk among patients with bladder cancer.
Despite the plethora of population-level studies (>20) to date suggesting an increased risk of suicidal death among cancer patients compared to the general population, all have failed to account for psychiatric care/psychiatric comorbidities before a cancer diagnosis, which may confound this relationship. In order to assess this discrepancy, Klaassen et al.14 assessed the effect of a cancer diagnosis on the risk of suicide, accounting for pre-diagnosis psychiatric care utilization using population-level data from Ontario for the ten most prevalent cancer types. As previously mentioned, a PUG score in the five years prior to a cancer diagnosis was calculated as follows: 0 – none; 1 – outpatient psychiatric utilization; 2 - emergency department psychiatric utilization; and 3 – psychiatric specific hospital admission. Noncancer controls were matched 4:1 based on sociodemographics, including the PUG score, and a marginal, cause-specific hazard model was used to assess the effect of cancer on the risk of suicidal death. Among 676,470 patients with cancer and 2,152,682 matched noncancer controls, there were 8.2 and 11.4 suicides per 1000 person-years of follow-up, respectively. Patients with cancer had an overall higher risk of suicidal death compared with matched patients without cancer (HR 1.34, 95% CI, 1.22-1.48). This effect was pronounced in the first 50 months after cancer diagnosis (HR 1.60; 95% CI, 1.42-1.81), whereas patients with cancer did not demonstrate an increased risk thereafter:

Furthermore, among individuals with a PUG score of 0 or 1, those with cancer were significantly more likely to die of suicide compared with controls. There was no difference in suicide risk between patients with cancer and controls for those who had a PUG score of 2 or 3, suggesting that among patients with severe psychiatric comorbidities the impact of a cancer diagnosis was less likely to increase risk of suicidal death. When specifically assessing bladder cancer patients versus non-cancer controls, the risk of suicidal death (accounting for pre-diagnosis psychiatric utilization of resources) was significantly higher (HR 1.73, 95% CI 1.14-2.62), with only lung cancer (HR 2.49, 95% CI 1.98-3.13) and oral cancer (HR 2.55, 95% CI 1.59-4.12) having a higher risk of suicidal death.
Bladder cancer patients have approximately a 70% increased risk of suicidal death compared to the general population/non-cancer controls. This increased risk is particularly pronounced among those that are male, elderly, white, unmarried, and those with non-localized disease. As such, early psychological support must be provided during the follow-up period of these special populations, as they may benefit from targeted survivorship plans.
Future Endeavors
Given the aforementioned data regarding the impact of depression, mental illness, and risk of suicide among bladder cancer patients, the time for prospective intervention and assessment of intervention efficacy among these patients is now.15 Bessa et al.16 performed a systematic review as part of the Medical Research Council Framework for developing complex interventions, providing an overview of the published mental wellbeing interventions that could be used to design an intervention specific for bladder cancer patients. A total of 15,094 records were collected from the search and 10 studies matched the inclusion and exclusion criteria. Of these, nine interventions were for patients with prostate cancer and one for patients with kidney cancer; no studies were found for other urological cancers. Depression was the most commonly reported endpoint measured, and of the included studies with positive efficacy, three were group interventions and two were couple interventions. In the group interventions, all studies showed a reduction in depressive symptoms, and in the couple interventions, there was a reduction in depressive symptoms and a favorable relationship cohesion.
Patient education and rehabilitation programs have also been tested prospectively among bladder cancer patients. Li et al.17 assessed the impact of this program on anxiety, depression, and quality of life in 130 muscle-invasive bladder cancer patients undergoing adjuvant chemotherapy. Patients were randomized 1:1 to the patient education and rehabilitation program group and to the control group. HADS anxiety and depression scores and QLQ-C30 scores were assessed before treatment and after treatment (week 16). They found that after 16 weeks of treatment the patient education and rehabilitation program group exhibited decreased HADS anxiety score (p = 0.036), ΔHADS anxiety score (between week 16 and week 0) (p < 0.001), and percentage of anxiety patients (p = 0.019) compared to control group. With regards to depression outcomes, the patient education and rehabilitation program group presented with numerically reduced HADS depression score (p = 0.076) compared to control group, as well as lower ΔHADS depression score (between week 16 and week 0) (p = 0.014) and percentage of depressed patients (p = 0.015). For quality of life, QLQ-C30 global health status score (p = 0.032), Δglobal health status score (between week 16 and week 0) (p = 0.003), and Δfunctional score (between week 16 and week 0) (p = 0.005) were higher in the patient education and rehabilitation program group compared to control group. However, no difference of QLQ-C30 functional score (p = 0.103), QLQ-C30 symptom score (p = 0.808) or Δsymptom score (between week 16 and week 0) (p = 0.680) was observed between two groups.
As urologic oncologists, we are not specifically trained to treat depression and mental health disorders in our bladder cancer patients, however, identifying risk factors and making appropriate consultations to psycho-oncologists is necessary. To further assess this, Mani et al. evaluated the prevalence of mental distress in patients with newly diagnosed bladder cancer, cancer-information internet search behavior, and the influence of information seeking on level of distress. For this study, 101 bladder cancer patients answered the HADS and Fragebogen zur Belastung von Krebskranken (FBK-R23) questionnaires in order to evaluate mental distress and assess questions concerning information seeking. Analysis of mental distress showed that 23.2% had a score above the HADS-A cutoff, 25.3% above the HADS-D cutoff, and 21.4% showed a pathologic FBK-R23 score. Overall, 75% felt well informed about their illness, and active searches for information/ use of the internet did not correlate with the HADS-A, HADS-D, or FBK-R23 score. However, the quality of the urologist's information and the feeling of being informed correlated with the grade of mental distress.
Besides the treatment of bladder cancer, informing patients about their disease in a psychologically wholesome manner and working together with psycho-oncologically trained psychologists are essential tasks for the treating urologist. Furthermore, future studies assessing interventions for improving mental health and outcomes among bladder cancer patients is crucial to identifying impactful interventions and monitoring strategies. Early work suggests that patient education and rehabilitation programs may be helpful in decreasing depression and anxiety among patients with bladder cancer.
Conclusions
Bladder cancer patients are a comorbid population. While often under-appreciated, many patients with bladder cancer have a pre-existing psychiatric diagnosis at the time of cancer diagnosis, and many others will develop mental health disorders after diagnosis. In addition to decreasing quality of life, previous studies have suggested that psychiatric comorbidities can negatively impact cancer-specific and overall survival. Additionally, bladder cancer patients are at a ~70% increased risk of suicidal death compared to the general population/non-cancer patients. While awareness of the importance of mental health in bladder cancer patients is growing, further studies are needed to assess the role of interventions such as cognitive-behavioral therapy or pharmacotherapy in order to optimize treatment.
Published Date: June 2021


