Introduction
Intravesical Bacillus Calmette-Guerin (BCG) remains the current standard-of-care, guideline-recommended treatment of choice in the adjuvant setting for intermediate- and high-risk non-muscle invasive bladder cancer (NMIBC) due to its ability to reduce the risk of disease recurrence and, more importantly, disease progression.1-3 Despite adequate BCG treatment up to 50% of patients will develop a BCG-refractory, relapsing, or failure state.4 Over the last several years, there has been a plethora of data in the BCG unresponsive disease space, leading to FDA approvals for pembrolizumab in January 2020 and nadofaragene firadenovec in December 2022.6 Many of these novel immune-based treatments overcome some of the limitations of older agents in this setting,7 particularly those related to short durations of exposure limiting their efficacy.8 This same concept of extending the intravesical exposure time has recently been extrapolated to the intravesical chemotherapeutic treatment landscape, where we have witnessed the emergence of novel agents with prolonged mechanisms of action and alternate methods of administration. In this Center of Excellence article, we will discuss the currently available evidence and ongoing studies for intravesical chemotherapeutic agents and photodynamic therapy in the BCG unresponsive NMIBC disease space.
Gemcitabine + Docetaxel
In 2020, the results of a multicenter, retrospective analysis evaluating sequential gemcitabine plus docetaxel in patients with recurrent NMIBC and a history of intravesical BCG treatment were reported. In this study, all patients received intravesical gemcitabine (1 gm/50 ml sterile water or saline) for 60 to 90 minutes, after which it was drained and intravesical docetaxel (37/5 mg/50 ml saline) was instilled and held for 1-2 hours. To minimize side effects secondary to the irritative effects of gemcitabine (pH 2.5), 1,300 mg of oral sodium bicarbonate was given the evening before and the morning of each instillation to alkalinize the urine. The induction regimen was given once weekly for 6 weeks, followed by monthly maintenance for up to 24 months in the majority of the participating institutions. Surveillance was performed in accordance with institutional/national guidelines.This analysis included 276 patients with a median age of 73 years. The median number of prior BCG courses was 2 (range: 1 to 8), with 38% of patients meeting the BCG unresponsive disease definition. From an efficacy standpoint, the 1- and 2-year recurrence-free survival rates were 60% and 46%, respectively, with similar recurrence rates observed for patients with CIS versus papillary-only disease. The high-grade recurrence-free survival rates in the overall cohort at 1 and 2 years were 65% and 52%, respectively:

Among patients with BCG unresponsive disease, the 2-year high-grade recurrence-free survival rates were 50% and 58% for CIS and papillary disease-alone cases, respectively:

Overall, 43/276 patients (15.6%) underwent a radical cystectomy, at a median follow-up of 11.3 months, and 11 patients (4%) had evidence of progression to muscle invasive disease. The most common side effects were frequency/urgency and dysuria, with 41% of patients reporting symptoms during treatment, but only 9.3% having symptoms that impacted the treatment schedule. There were no reported treatment-related deaths.9
Long-term follow-up of a subset of this cohort from the University of Iowa was recently published in 2023. This analysis included 97 patients (35% BCG unresponsive), with a median follow-up of 49 months. The 3-month complete response rate was 74%, with a median duration of response of 25 months. The high-grade recurrence-free survival rates were:
- 1 year: 60%
- 2 years: 50%
- 5 years: 30%
Device-assisted Administration of Intravesical Chemotherapy
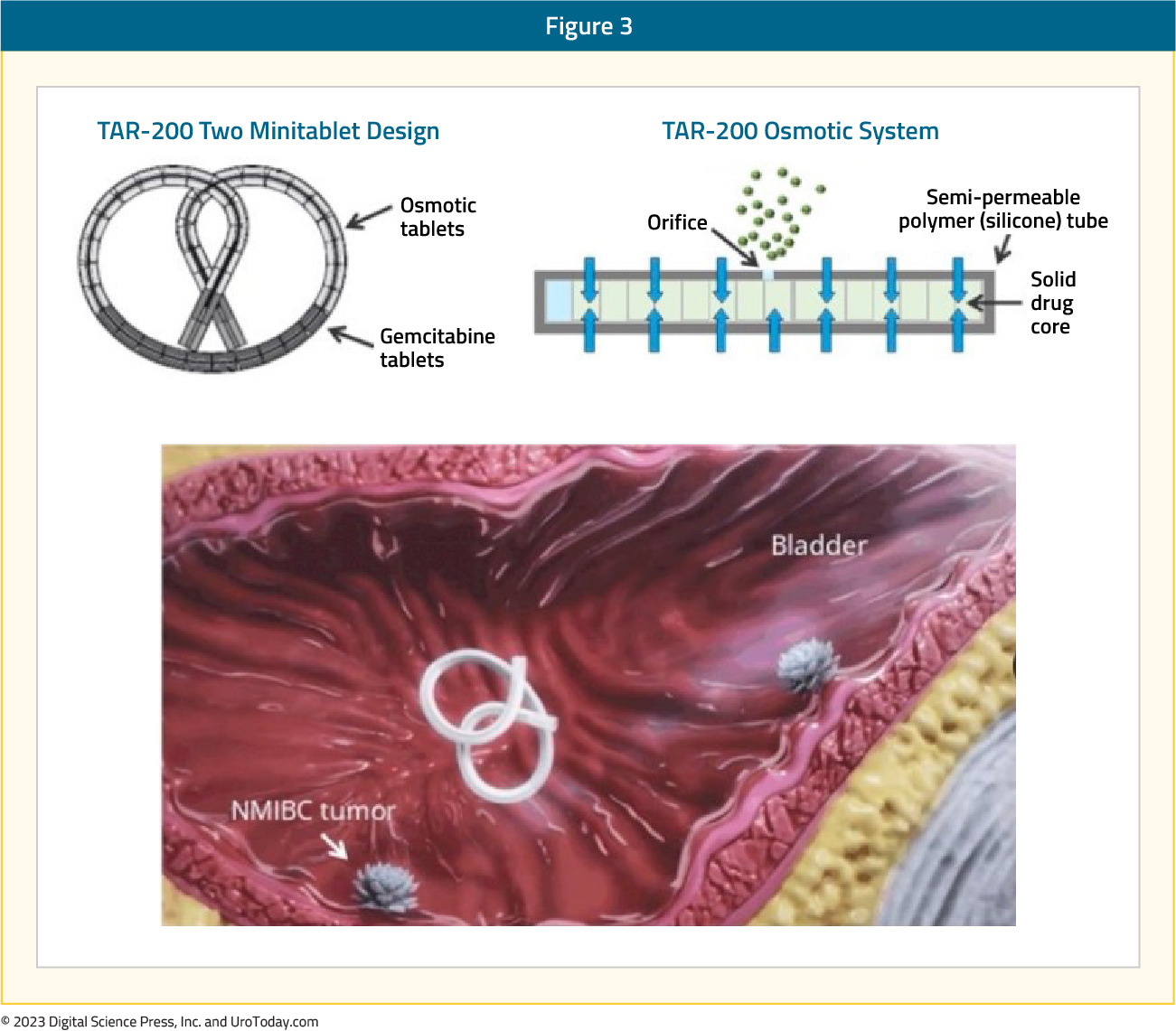
TAR-200TAR-200/gemcitabine (JNJ-17000139) is a novel drug delivery system that allows for the sustained local release of gemcitabine intravesically, relying on an osmotic system as illustrated below:
Evaluation of urine and plasma gemcitabine concentrations over a 7-day period demonstrates the ability of TAR-200 to provide sustained, local delivery of gemcitabine while limiting systemic toxicity. As demonstrated in the figure below, intravesical instillation of gemcitabine (green curve) is associated with a sharp increase/decrease in the gemcitabine urine concentration, which is non-sustained beyond day 1. Conversely, we see an increase in the urinary gemcitabine concentration between days 1 and 3 with TAR-200 (blue curve), followed by a gradual decline with measurable levels detected until at least day 7. Importantly, no gemcitabine is detected in the plasma of patients receiving TAR-200.

SunRISe-1 is a randomized trial of BCG-unresponsive, high-risk NMIBC patients with CIS +/- papillary disease, who did not receive a radical cystectomy. Patients underwent stratified randomization (by presence or absence of concomitant papillary disease) in a 2:1:1 fashion to either:
- Cohort 1: TAR-200 + cetrelimab (PD-1 inhibitor)
- Cohort 2: TAR-200 alone (target sample size 50, currently enrolled: 23)
- Cohort 3: Cetrelimab alone (target sample size 50, currently enrolled: 24)
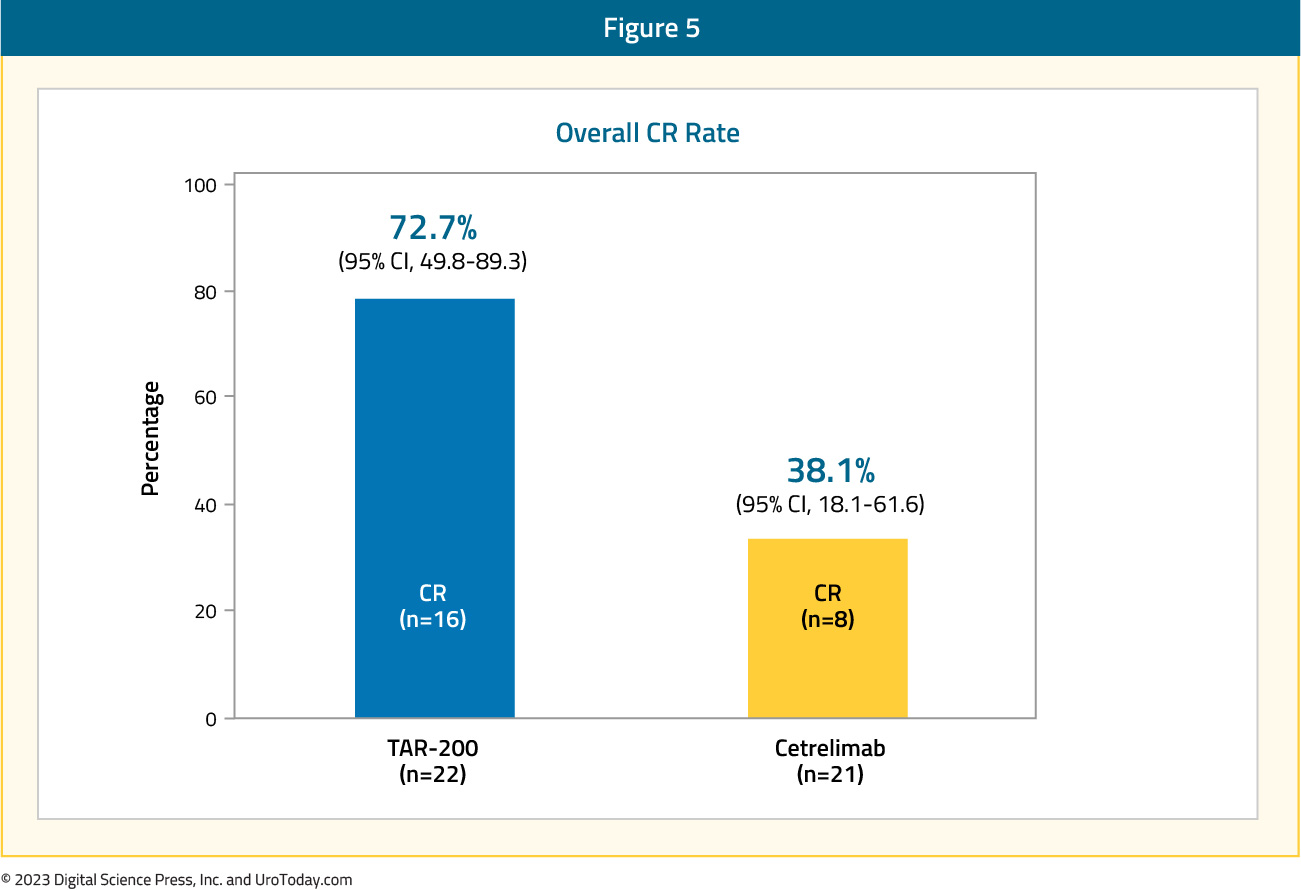
The median patient age was 70 – 72 years, pure CIS was present in 70% and 65% of patients in the TAR-200 and cetrelimab groups, respectively, and the median total doses of prior BCG were 12 in each arm. From an efficacy standpoint, 73% of patients in the TAR-200 arm achieved a complete response (median duration of response not yet reached), defined based on the results of cystoscopy, centrally assessed urine cytology, and mandated biopsy at weeks 24 and 48. The CR rate in the cetrelimab arm was 38%.
Overall, most adverse events in the TAR-200 group were grade ≤2, with those reported in the cetrelimab group similar to that expected and observed with other PD-1 agents. 9% and 4% of patients discontinued TAR-200 and cetrelimab due to treatment-related adverse events. In each arm, 1 patient had treatment-related serious adverse events and 2 patients had treatment-related grade ≥3 adverse events. No deaths were observed in the study.11

Given these promising findings from the TAR-200 monotherapy arm, Janssen announced that they will be suspending further enrollment to the TAR-200 + cetrelimab arm.
Radiofrequency-induced Thermochemotherapy
In 2009, the results of a multi-institutional analysis of 51 patients from 15 European centers receiving mitomycin combined with intravesical hyperthermia in patients with mainly BCG-failing CIS (35/51) were published. Patients received mitomycin via the Synergo® system SB-TS 101, which uses an intravesical microwave applicator to deliver hyperthermia to the bladder wall via direct irradiation, weekly for 6–8 weeks, followed by 4–6 sessions every 6–8 weeks. Of 49 evaluable patients, there was evidence of a complete CIS response (negative biopsy and cytology) at 3 months in 45 patients (92%). Patients had similar outcomes irrespective of whether they met the BCG failure definition or not. Among the 45 responders, 49% had a recurrence at a median follow-up of 22 months. The most common adverse events were bladder spasms (13.1%), pain (12.7%), and dysuria (6.2%), and were generally mild in severity.12A follow-up analysis of 150 patients who received ≥6 radiofrequency mitomycin instillations (induction and maintenance) was reported in 2018. All included patients had either pathology or cystoscopy plus cytology available at 6 months of follow-up. Of these 150 patients, 50 (33.3%) had BCG-unresponsive disease, with a 6-months complete response rate of 36% in this subgroup. The two-year recurrence-free survival rate was 82.6%, with a three-year cystectomy-free rate of 71.4%. Treatment discontinuation due to adverse events occurred in 13.4% of patients receiving induction treatment and 17.8% of those receiving maintenance instillations.13
Hyperthermic Intravesical Chemotherapy
In 2018, de Joeng et al. reported the results of hyperthermic intravesical chemotherapy (HIVEC) in 52 patients with BCG unresponsive NMIBC. Patients received intravesical instillations of mitomycin (80 mg in 50 mL of distilled water) that were extravesically heated up to 41-43°C and recirculated during 60 minutes at 200 m/min at stable pressure. All instillations were conducted with the Combat BRS system V2.0. The 3-months complete response rate was 75%. By 12 months follow-up, 47% of patients had remained disease-free. The overall median disease-free survival was 17.7 months and was significantly longer in those with papillary disease at 28.8 months versus 17.7 months in those with CIS. Patients in the ‘very high risk’ BCG unresponsive group had the shortest disease-free survival duration at 12.1 months. Any adverse event was reported in 69% of patients, with almost all grade 1-2 in severity, most common of which was urinary frequency/urgency (35%), urinary tract pain (15%), and bladder spasms (7%).14
In 2022, results of the multi-institutional Hyperthermic Chemotherapy registry (HIVEC-E) were published. These included a total of 1,028 patients, with 172 (21%) and 74 (9%) having disease classified as BCG unresponsive and failure, respectively. The 12- and 24-months recurrence-free survival rates for the BCG unresponsive cohort were 78.1% and 57.4%, respectively. Among patients in the BCG unresponsive cohort, the 24-months recurrence-free survival rates were superior for those papillary only disease (64.5% versus 43.6% for those with CIS). Minor and severe adverse events occurred in 26% and 2% of patients, respectively.15
Photodynamic Therapy
TLD-1433 is a novel ruthenium-based photosensitizer that selectively binds to bladder cancer cells. When activated by a 520 nm intravesical laser (TLC-3200) under general anesthesia (90 J/cm2 of laser light), it generates cytotoxic singlet oxygen and radical oxygen species, leading to cell death. PDT is also known to induce an antitumor cascade of immune signaling.16,17
At ASCO GU 2023, Dr. Girish Kulkarni presented the interim results of a phase II trial evaluating this intravesical photo dynamic therapy in patients with BCG unresponsive CIS. At the time of presentation, the trial had enrolled 52 patients (70% pure CIS, 20% CIS + HG T1, 10% CIS + Ta). This was a heavily pre-treated cohort, with 21% having >19 prior BCG instillations. A complete response, defined by a negative cystoscopy and cytology, was observed in 54% of patients. Among the 12 patients who had available follow-up at 450 days, 8 (67%) had a complete response. While 9/52 patients experienced a serious adverse event, none were deemed directly treatment-related per the Data Safety Monitoring Board.18
Enfortumab Vedotin
Enfortumab vedotin (EV) is a Nectin-4 targeted antibody-drug conjugate. Nectin-4 is highly expressed on bladder tumor cells, making it an attractive target for such agents. Systemic use of EV has previously demonstrated an overall survival benefit in the 3rd line setting for patients with locally advanced or metastatic urothelial carcinoma, who had previously received platinum-based therapy and a PD-1 or PD-L1 inhibitor (EV-301).19 Based on its demonstrated benefit in locally advanced/metastatic urothelial carcinoma, EV is currently being evaluated in earlier settings. EV-104 (NCT05014139) is a phase 1, open-label, multicenter, dose-escalation, and dose-expansion study of intravesical EV in adults with high-risk BCG-unresponsive NMIBC (CIS +/- papillary disease) who are ineligible for or refuse radical cystectomy. The primary study objectives are to evaluate the safety and tolerability of intravesical EV and determine the maximum-tolerated and recommended phase II doses of intravesical EV.Similar in concept to BCG and intravesical chemotherapy regimens, the EV-104 treatment regimen will include an induction phase, whereby patients will receive intravesical EV weekly for 6 weeks followed by monthly maintenance for a total of 9 additional EV doses. Patients will undergo cystoscopy and cytology every 3 months and annual upper tract imaging.

The study is currently enrolling in the United States (since January 2022) with additional sites planned in Canada and Europe, including the UK.
Erdafitinib
Erdafitinib is an oral selective pan-fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor that is approved for locally advanced or metastatic urothelial carcinoma in adults with FGFR3/2 alterations who have progressed during or after at least one line of platinum-containing chemotherapy.20 THOR-2 is a multi-cohort, phase II trial of erdafitinib in patients with high-risk NMIBC, with Cohort 2 including patients with BCG-unresponsive CIS (+/- papillary disease) and FGFR3/2 alterations. In this cohort, patients received continuous oral erdafitinib 6 mg once daily.Interim results were presented at ASCO GU 2023 by Dr. James Catto. At time of presentation, Cohort 2 had enrolled 10 patients with a median age of 72 years. The complete response rates at the 1st (Cycle 3, Day 1) and 2nd evaluations (Cycle 6, Day 1) were 100% and 75%, respectively. At a median follow-up of 10 months, the median duration of response was 3.0 months. Grade 3 or worse treatment-related adverse events occurred in 3 patients (30%), and included dry mouth, stomatitis, nail disorder, onychomadesis, acute kidney injury, chronic kidney disease, sepsis, and hypotension. One patient discontinued treatment due to adverse events. There were no treatment-related deaths.
Conclusions
Intravesical chemotherapeutic agents have emerged as promising treatment options for patients with BCG unresponsive NMIBC. Given its ease of administration and wide availability, the intravesical combination of gemcitabine plus docetaxel has emerged as one of the most commonly used treatments in this setting in clinical practice. TAR-200, via a local sustained release of gemcitabine, demonstrates excellent early response rates in SunRISE-1. These agents add to the growing armamentarium in the BCG unresponsive disease space with future regulatory approvals by the FDA contingent on further follow-up of current and future studies of these agents.
Published September 2023


